Understanding Medical Coding Anesthesia and Billing: Guidelines, Tips, and Best Practices
Anesthesia coding and billing are critical components of the healthcare reimbursement process, ensuring that anesthesia services are properly compensated for the care provided to patients during procedures and surgeries. Given the complexity of anesthesia services and the unique set of codes used, it is essential for medical coders and billers to understand the intricacies involved. This blog will explore the key principles of medical coding anesthesia, common billing guidelines, and helpful tips to ensure accurate and efficient claims processing.
What is Medical Coding Anesthesia?
Anesthesia coding refers to the process of assigning the correct codes to anesthesia services provided to patients. These services can range from local anesthesia for minor procedures to general anesthesia for major surgeries. Anesthesia coding requires knowledge of both the CPT (Current Procedural Terminology) codes and the ICD-10-CM diagnosis codes, as well as the specific rules surrounding anesthesia services, including time-based coding, modifiers, and physical status classification.
Key Components of Medical Coding Anesthesia
CPT Codes for Anesthesia Services: The CPT code for anesthesia services is typically a five-digit code, starting with a “0” (e.g., 00100-01999). These codes correspond to the different types of anesthesia used during specific procedures. For example:
- 00100-01999: Anesthesia codes for various surgical procedures
- 01916: Anesthesia for major vascular surgery
- 00840: Anesthesia for eye surgery
Each anesthesia code corresponds to a particular procedure or surgical site, and these codes should be selected based on the surgery the patient is undergoing.
Physical Status Modifiers (P1-P6): Physical status modifiers are used to provide additional information about the patient’s overall health status and how it might impact anesthesia risk. These modifiers are added to the anesthesia code to help reflect the patient’s physical condition. The six physical status modifiers are:
- P1: A normal healthy patient
- P2: A patient with mild systemic disease
- P3: A patient with severe systemic disease
- P4: A patient with severe systemic disease that is a constant threat to life
- P5: A patient who is not expected to survive without the operation
- P6: A declared brain-dead patient whose organs are being removed for donation
The use of these modifiers helps determine the complexity and risk of the anesthesia provided, which can affect the reimbursement rate.
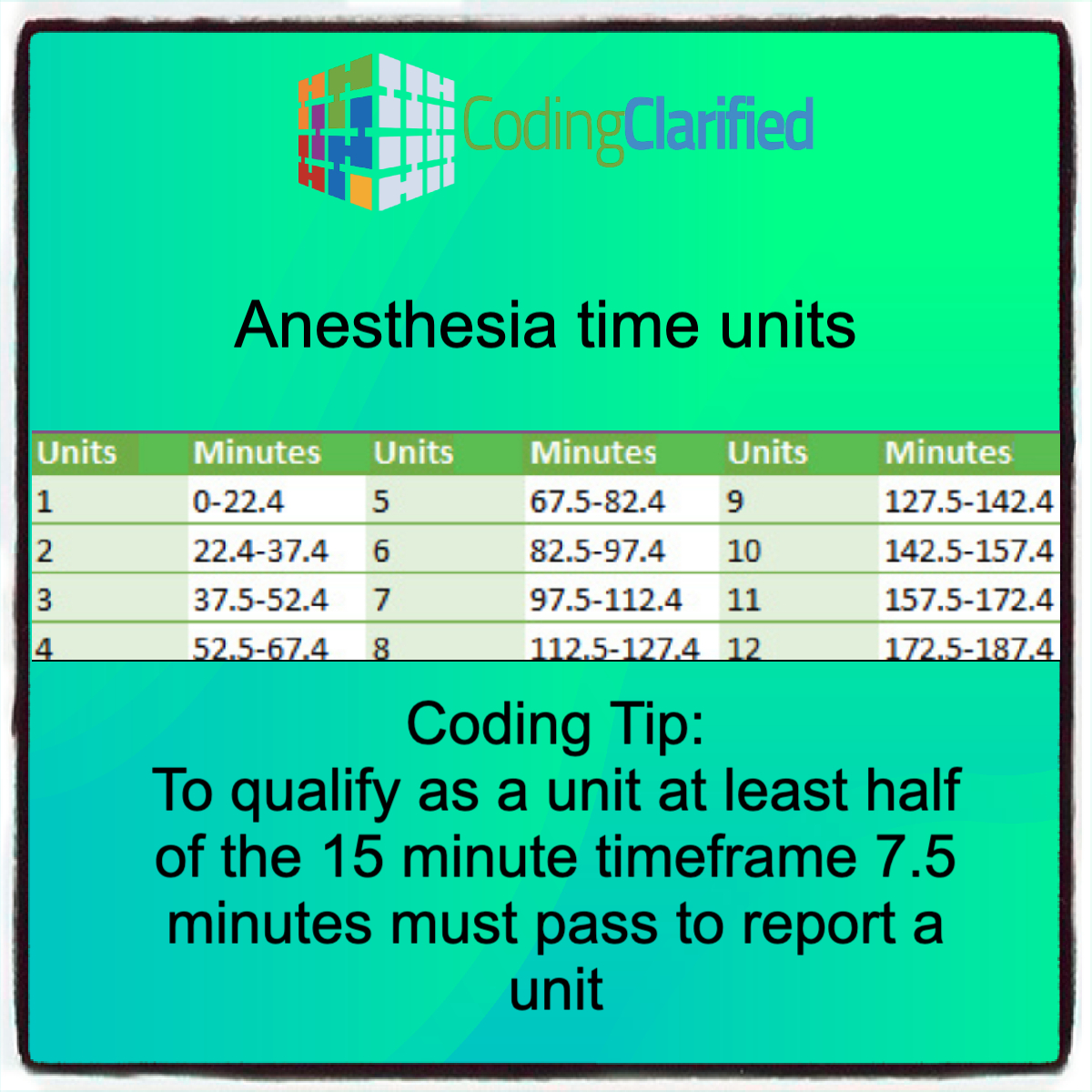
Time-Based Billing: Anesthesia services are generally billed based on the time spent providing anesthesia care. This includes the time from the moment the anesthesia provider begins to prepare the patient for anesthesia until the patient is safely transferred to the post-anesthesia care unit (PACU). The time is typically calculated in 15-minute increments.
Basic rule: Anesthesia time is billed using a “units” system, where each unit typically corresponds to 15 minutes of anesthesia care.
Example: If anesthesia is administered for 60 minutes, it would be billed as four units.
Add-on Codes for Special Services: In some cases, additional services related to anesthesia are required. These may include the administration of anesthesia in special circumstances (e.g., for epidurals or labor anesthesia). Add-on codes (e.g., 01967 for labor anesthesia) are used to bill these services, and they should always be used in conjunction with the primary anesthesia code.
ICD-10-CM Diagnosis Codes for Anesthesia
In addition to the CPT anesthesia codes, appropriate ICD-10-CM diagnosis codes must be used to describe the underlying condition for which the anesthesia is administered. For instance:
- If a patient is undergoing surgery due to appendicitis, the diagnosis code for appendicitis (e.g., K35.80 for acute appendicitis) should be listed.
- If anesthesia is being administered due to a trauma-related condition, the relevant trauma codes must be included.
The ICD-10-CM code helps link the anesthesia service to the patient’s medical condition, ensuring that the service is medically necessary and justifying the use of anesthesia for the procedure.
Anesthesia Billing Guidelines
Proper billing for anesthesia services is essential for avoiding delays in payment or claim denials. Below are some important anesthesia billing guidelines:
Correct Coding for Procedure and Anesthesia Type: It’s important to ensure that the anesthesia code reflects the type of procedure performed. For example, different types of surgeries (e.g., orthopedic, abdominal, or cardiovascular) require specific anesthesia codes. Verify that the anesthesia service corresponds to the correct surgical procedure.
Modifiers:
- Modifier 23: Used for unusual anesthesia (e.g., anesthesia administered during an emergency or unusually prolonged procedures).
- Modifier 47: Used to indicate that the anesthesia was administered by the surgeon rather than an anesthesiologist (rarely used but necessary in some situations).
- Modifier AA: Indicates that anesthesia services were performed by the anesthesiologist personally.
- Modifier QK: Indicates that the anesthesia service was performed by an anesthesiologist in a teaching hospital with supervision.
Using the correct modifiers ensures that claims are processed correctly and reimbursements are maximized. CPT Modifiers https://codingclarified.com/cpt-medical-modifiers/
Anesthesia Time Calculation: Accurately documenting the time spent administering anesthesia is crucial for proper billing. Ensure that the anesthesia time is calculated from the moment the anesthesia is first administered to the point when the anesthesia care ends. Round time to the nearest 15-minute increment for billing. Medicare 8 Minute Rule https://codingclarified.com/medicare-8-minute-rule/
Documentation and Medical Necessity: Adequate documentation is key for anesthesia billing. The anesthesia provider should document the type of anesthesia used, the time spent, the physical status of the patient, and any other special services provided (e.g., additional monitoring or use of special equipment). The medical record must support the medical necessity of anesthesia for the procedure.
Billing for Multiple Anesthesia Providers: When more than one anesthesia provider is involved in the procedure (e.g., a CRNA working under the supervision of an anesthesiologist), there may be a split or shared anesthesia code. The roles of the providers should be clearly documented, and the appropriate modifier should be used to indicate whether the anesthesiologist or CRNA provided the primary anesthesia care.
Tips for Accurate Medical Coding Anesthesia and Billing
Ensure Proper Documentation of Anesthesia Time: Document the start and end times of anesthesia administration in the patient’s medical record to ensure correct time-based billing. Failure to document time accurately can result in denied claims or under-reimbursement.
Always Use the Correct Physical Status Modifier: Choose the correct modifier based on the patient’s health condition. This modifier provides insight into the complexity of the anesthesia and ensures appropriate reimbursement for the risk involved.
Review the Anesthesia Procedure and Diagnosis Codes: Always double-check the procedure being performed and the diagnosis to ensure that the correct anesthesia code is selected. Anesthesia codes are specific to the type of surgery and the patient’s condition.
Avoid Upcoding or Downcoding: Never overestimate or underestimate the anesthesia time or complexity. Both upcoding and downcoding can lead to problems with reimbursements and audits. Stick to the exact number of units based on time spent providing anesthesia care. Bundling and Upcoding https://codingclarified.com/medical-coding-bundling-and-upcoding-guidelines/
Stay Up-to-Date on Changes: Anesthesia billing codes and guidelines may change, so it’s important for coders and billers to stay informed about updates to the CPT and ICD-10 coding systems, as well as any payer-specific billing requirements.
Know the Payer Guidelines: Different insurance carriers and government programs (like Medicare) may have specific guidelines for billing anesthesia services. Ensure you are familiar with payer-specific requirements to avoid denials or underpayment.
Anesthesia coding and billing require attention to detail and a solid understanding of both the clinical and administrative aspects of anesthesia services. By using accurate codes, applying the correct physical status modifiers, and ensuring proper documentation of anesthesia time and patient status, medical coders and billers can maximize reimbursement and reduce the likelihood of claim denials. Following the guidelines and tips provided in this blog will help ensure that anesthesia claims are processed efficiently and accurately, ensuring proper compensation for anesthesia providers.