Upcoding and Bundling Guidelines for Coders and Billers: Ensuring Accurate and Ethical Billing Practices
In the healthcare industry, accurate medical coding and billing are essential to ensure that healthcare providers receive appropriate reimbursement for services rendered while also adhering to regulatory and ethical standards. Two practices that often lead to confusion and potential compliance issues are medical coding bundling and upcoding. This blog aims to explain these concepts and provide guidelines for medical coders and billers to avoid errors and ensure compliance with relevant healthcare policies.
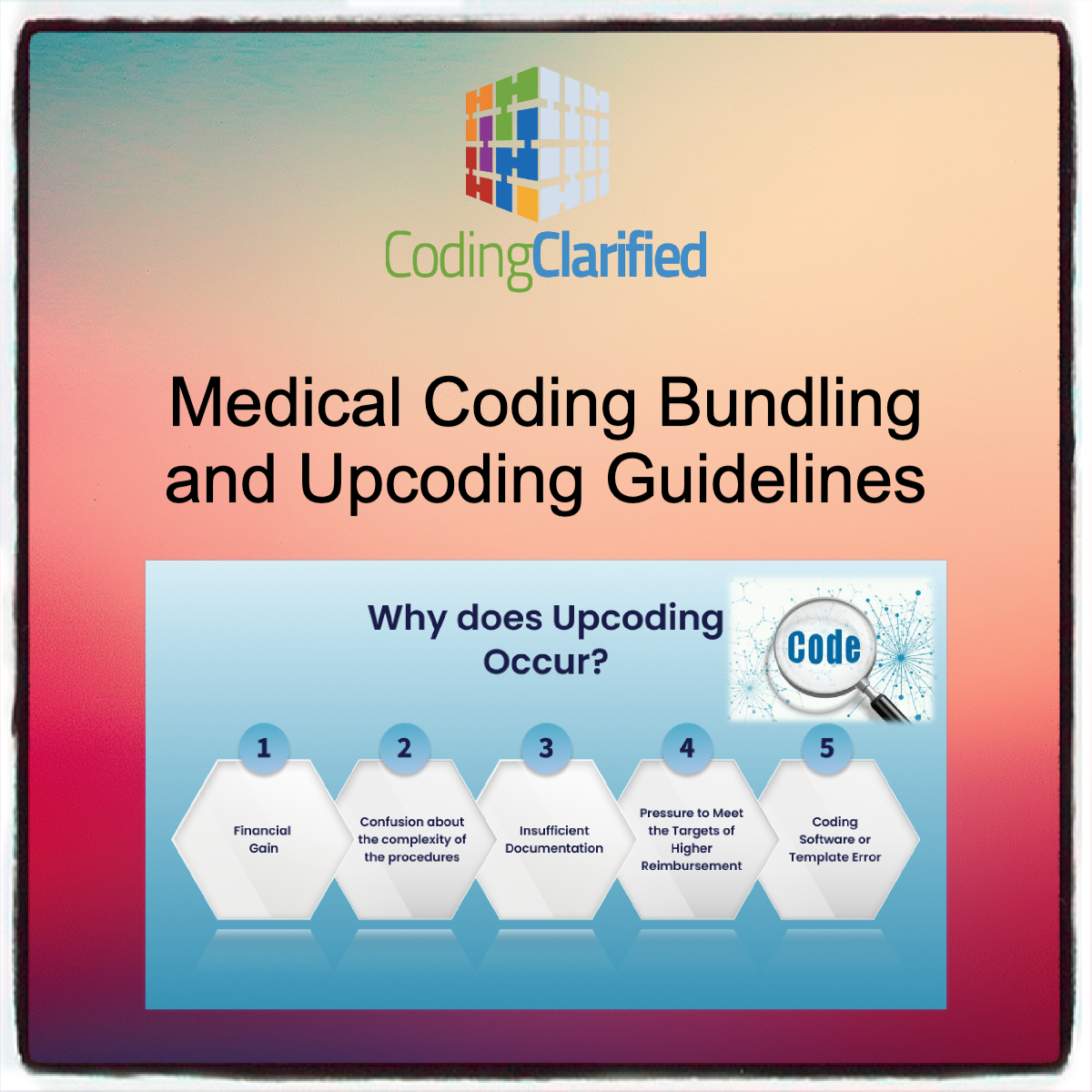
What is Upcoding?
Upcoding refers to the practice of submitting a healthcare claim that inaccurately represents the level of services or procedures provided, often to increase reimbursement. Upcoding can occur in a variety of ways, such as assigning a higher-level procedure or diagnosis code than what was actually performed or diagnosed.
Common Examples of Upcoding:
- Selecting a higher-level E&M (Evaluation and Management) code for a routine office visit when a lower-level code would be more appropriate.
- Misrepresenting the complexity of a procedure by coding for a more extensive surgery when a less complex procedure was performed.
- Coding for a more severe diagnosis than what was documented in the patient’s medical record, leading to increased reimbursement.
Why Upcoding is Problematic
Upcoding is considered fraud by the Centers for Medicare & Medicaid Services (CMS) and other insurers because it results in overpayments, which ultimately contribute to higher healthcare costs. It can also lead to legal and financial consequences for healthcare providers, including fines, audits, and the loss of accreditation.
What is Bundling?
Bundling refers to the practice of grouping multiple services or procedures together under a single code, often resulting in a lower reimbursement than if each service was billed separately. It’s a legitimate practice that is commonly used in healthcare billing, particularly for related procedures that are typically performed together.
Bundling Examples:
- Global Surgery Codes: These codes bundle together the various components of a surgical procedure, such as preoperative visits, the surgery itself, and postoperative care. For example, CPT code 99354 (Prolonged office visits) may not be reported separately during a surgery follow-up since it is bundled into the global surgical code.
- Laboratory Services: If a patient undergoes a series of related lab tests, a bundled payment may cover the entire diagnostic workup instead of individual payments for each test.
Bundling Guidelines
- National Correct Coding Initiative (NCCI): The NCCI guidelines are used by Medicare and other insurers to determine which services or procedures are considered bundled. Coders must check NCCI edits to ensure that they are not improperly billing services that are bundled together.
- Medically Necessary and Reasonable: Even when bundling is required, the bundled services must be medically necessary and documented as part of a legitimate treatment plan.
- Modifiers: In some cases, coders can use specific modifiers (like Modifier 59) to report separate services that would typically be bundled together when they are performed independently or in different situations.
Upcoding and Bundling: Ethical and Compliance Considerations
Ethical Guidelines for Medical Coders and Billers
Both upcoding and bundling require careful attention to documentation and coding guidelines to ensure compliance. Coders and billers must:
- Follow Documentation Requirements: The code selected must always match the documentation in the patient’s medical record. Accurate coding starts with detailed and complete documentation.
- Ensure Transparency: If any services are separately identifiable and not subject to bundling, coders must flag them and ensure they are billed correctly.
- Avoid Misrepresentation: Coders should never select codes based on reimbursement rates or financial incentives. Codes should reflect the actual care delivered.
Remote Medical Coding and AAPC Code of Ethics https://codingclarified.com/remote-medical-coding-ethics/
Compliance with Regulatory Agencies
Both the Health Insurance Portability and Accountability Act (HIPAA) and the False Claims Act make it illegal to submit claims based on fraudulent coding, whether through upcoding or improper bundling. The Office of Inspector General (OIG) and CMS conduct regular audits to ensure compliance with coding and billing rules. Violating these rules can lead to severe penalties, including fines, exclusion from federal healthcare programs, and criminal charges.
Guidelines for Avoiding Upcoding and Improper Bundling
Review the Medical Record Thoroughly
Ensure that all documentation supports the service codes being used. If the documentation does not clearly justify the level of service or procedure, it may be considered upcoding to select a higher-level code.
Utilize Official Coding Resources
Coders should use the Current Procedural Terminology (CPT) codes, International Classification of Diseases (ICD-10) codes, and Healthcare Common Procedure Coding System (HCPCS) codes accurately. It’s also essential to stay up-to-date with changes in these systems and billing policies through CMS, the American Medical Association (AMA), and other reliable sources.
Understand Bundling Rules
Coders should always be aware of which services or procedures are bundled together. The NCCI Edits are an essential tool in understanding bundling rules. These edits prevent inappropriate billing of services that are typically bundled together.
Use Modifiers Correctly
Modifiers such as Modifier 59 (Distinct procedural service) and Modifier 51 (Multiple procedures) can sometimes be used to unbundle services when appropriate, but coders should use them sparingly and only when warranted by the clinical situation.
CPT Medical Modifiers https://codingclarified.com/cpt-medical-modifiers/
Conduct Regular Training
Given the complexities of coding and billing practices, it is essential for healthcare organizations to provide ongoing training to coders and billers. This ensures they are familiar with the latest coding rules, upcoding and bundling practices, and compliance requirements.
Conduct Internal Audits
Regular audits of coding practices within a healthcare organization can help identify potential errors or patterns of upcoding or bundling violations. This can help catch mistakes early and prevent them from leading to claims denials or legal issues.
Upcoding and bundling are essential concepts in medical coding, but they require careful attention and strict adherence to regulatory guidelines. While upcoding is considered fraudulent and must be avoided at all costs, bundling is a legitimate practice that can lead to accurate and efficient billing, provided that coders and billers are fully aware of the applicable codes and rules. By staying informed, accurately documenting services, and following best practices for coding, medical coders and billers can contribute to ethical and compliant billing practices that safeguard both patient care and healthcare organizations’ financial integrity.
Read this from the AMA for more information: 8 medical coding mistakes that could cost you.