Guidelines & Tips for Distinguishing Acute vs Chronic in Medical Coding and Billing
Accurate medical coding and billing are vital aspects of healthcare management, ensuring that healthcare providers receive proper reimbursement for the services rendered. Distinguishing between acute vs chronic in medical coding is one critical aspect. This distinction is essential for proper coding, billing, and clinical documentation.
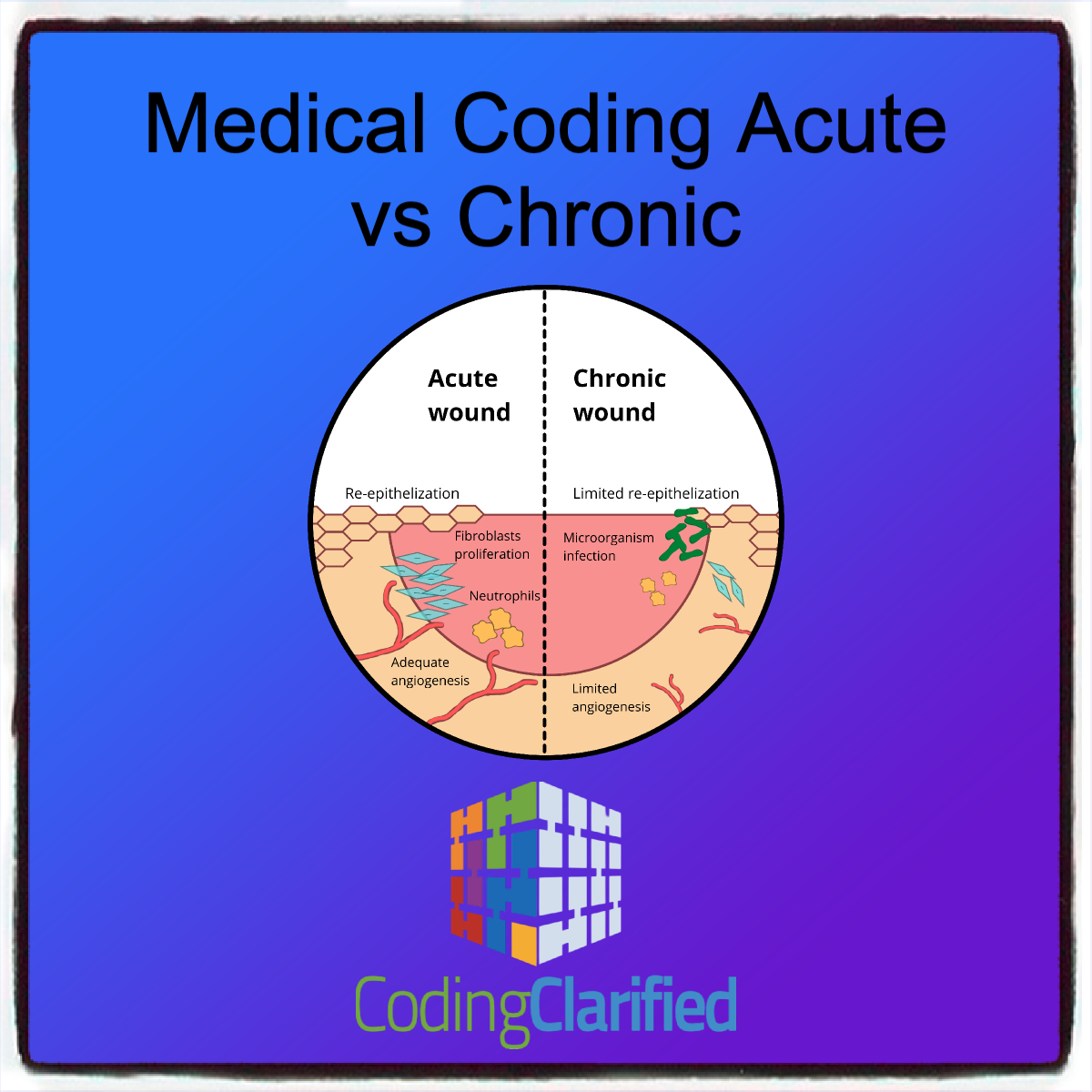
Understanding Acute vs Chronic Conditions
Before diving into the guidelines and tips, it’s important to understand what acute and chronic conditions are:
Acute Conditions: These conditions arise suddenly and have a short duration. They are typically severe but can be treated with interventions that lead to recovery. Examples include pneumonia, a heart attack, or a sprained ankle.
Chronic Conditions: These conditions develop over a long period and persist for months or even years. Chronic conditions may be manageable but often require ongoing treatment. Examples include diabetes, hypertension, and osteoarthritis.
Chronic Conditions https://codingclarified.com/medical-coding-for-chronic-conditions/
Medical Coding Guidelines for Acute vs Chronic Conditions
ICD-10-CM Codes:
Acute conditions are generally coded with acute disease codes in the ICD-10-CM (International Classification of Diseases, Tenth Edition, Clinical Modification) manual. These codes are specific to the type, location, and severity of the condition. For instance, pneumonia would be coded as an acute disease.
Chronic conditions, on the other hand, are coded under chronic disease codes. It’s important to note that many chronic conditions have a long-term nature and may require codes for both the condition itself and any associated complications (e.g., chronic kidney disease, diabetes with complications).
Secondary codes for complications: If a chronic condition leads to an acute exacerbation (e.g., acute exacerbation of chronic obstructive pulmonary disease or COPD), both the chronic condition and the acute exacerbation should be coded, as they are distinct entities.
Sequencing of Acute vs Chronic Conditions:
Acute conditions generally take precedence in coding, especially when a patient presents for treatment of the acute condition, even if they also have a chronic condition.
If a chronic condition is the primary focus of the treatment (e.g., a routine follow-up visit for diabetes management), the chronic condition should be listed as the primary diagnosis.
Exacerbations or complications of chronic conditions should be coded according to whether the exacerbation or complication is acute and requires more immediate attention. For example, a patient with diabetes who presents with diabetic ketoacidosis would have diabetes as the chronic condition, but diabetic ketoacidosis (an acute complication) would be listed first.
Sequencing https://codingclarified.com/medical-coding-sequencing/
Use of Z Codes:
When dealing with chronic conditions, especially during regular check-ups, Z codes (encounter codes) might be used in conjunction with chronic disease codes to indicate encounters for ongoing care (e.g., Z79.4 for long-term use of insulin in patients with diabetes).
In cases where chronic conditions are stable and not actively treated, you might code the chronic condition alone with a Z code, like Z51.81 for chemotherapy or radiation therapy.
Modifier Codes:
Modifier codes such as Modifiers 25 (Significant, Separately Identifiable Evaluation and Management Service) or Modifier 59 (Distinct Procedural Service) may be necessary when acute and chronic conditions are treated together during the same visit. These modifiers provide additional details for accurate billing and reimbursement.
CPT Modifiers https://codingclarified.com/cpt-medical-modifiers/
Billing Guidelines for Acute vs Chronic Conditions
Proper billing requires understanding the relationship between the patient’s condition and the treatment provided. Here are some key billing guidelines:
Acute Care Visits:
Acute conditions often result in higher reimbursement rates due to the nature of the services required (e.g., diagnostic testing, emergency services, and short-term treatment).
For acute conditions, the E/M (Evaluation and Management) code should reflect the complexity and time spent on care. If the patient is treated in an emergency department, level 1 to level 5 E/M codes may be applicable, depending on the severity of the acute condition.
Chronic Care Management (CCM) Services:
Chronic care management services involve continuous, non-acute treatment for ongoing conditions. These services may be billed under specific codes for long-term care or chronic care management (e.g., CPT codes 99490, 99439 for CCM).
For chronic conditions, healthcare providers should be aware of medically necessary services that are covered for long-term care, such as medication management, lab work, and monitoring for complications.
Preventive Services for Chronic Conditions:
Preventive services such as screenings, check-ups, and health risk assessments should be coded separately from treatment services for chronic conditions.
Preventive care codes (e.g., CPT codes 99381–99397) should be used for routine health check-ups related to chronic conditions, whereas chronic disease management codes should be used for ongoing treatment or monitoring.
Billing for Exacerbations:
When an acute exacerbation of a chronic condition occurs, it can affect both coding and reimbursement. The billing must reflect the fact that the acute condition (exacerbation) requires immediate care.
Providers should be sure to list both the chronic condition and the acute exacerbation to ensure proper reimbursement for both ongoing care and urgent interventions.
Tips for Accurate Coding and Billing
- Thorough Documentation: Always ensure that the clinical documentation provides clear and specific details of both acute and chronic conditions. This helps avoid coding errors and reduces the likelihood of claim denials.
- Stay Updated: Medical coding and billing rules change regularly, so it’s crucial to stay updated on any modifications to ICD-10, CPT, and HCPCS codes, especially those that pertain to acute and chronic conditions.
- Know the Guidelines for Exacerbations: When a patient’s chronic condition is complicated by an acute exacerbation, be sure to code both conditions properly and follow the correct sequencing guidelines.
- Educate Providers: Ensure that all healthcare providers are trained to document accurately and in detail. The more specific the diagnosis and treatment details, the easier it will be to apply the correct codes.
- Monitor Coding Audits: Regular audits of coded claims can identify any recurring issues with the coding of acute vs chronic conditions. Addressing these issues promptly can help avoid reimbursement issues.
- Use a Coding Specialist: A professional medical coder can help ensure that codes are accurate, compliant, and reflect the full scope of the patient’s condition and care.
The distinction between acute and chronic conditions is essential for accurate medical coding and billing. Understanding the guidelines and tips for coding these conditions correctly helps ensure that healthcare providers are appropriately reimbursed while also maintaining compliance with healthcare regulations. By focusing on precise documentation, correct code selection, and proper billing practices, healthcare organizations can streamline their revenue cycle and avoid costly claim denials.
https://www.ncoa.org/article/chronic-versus-acute-disease/