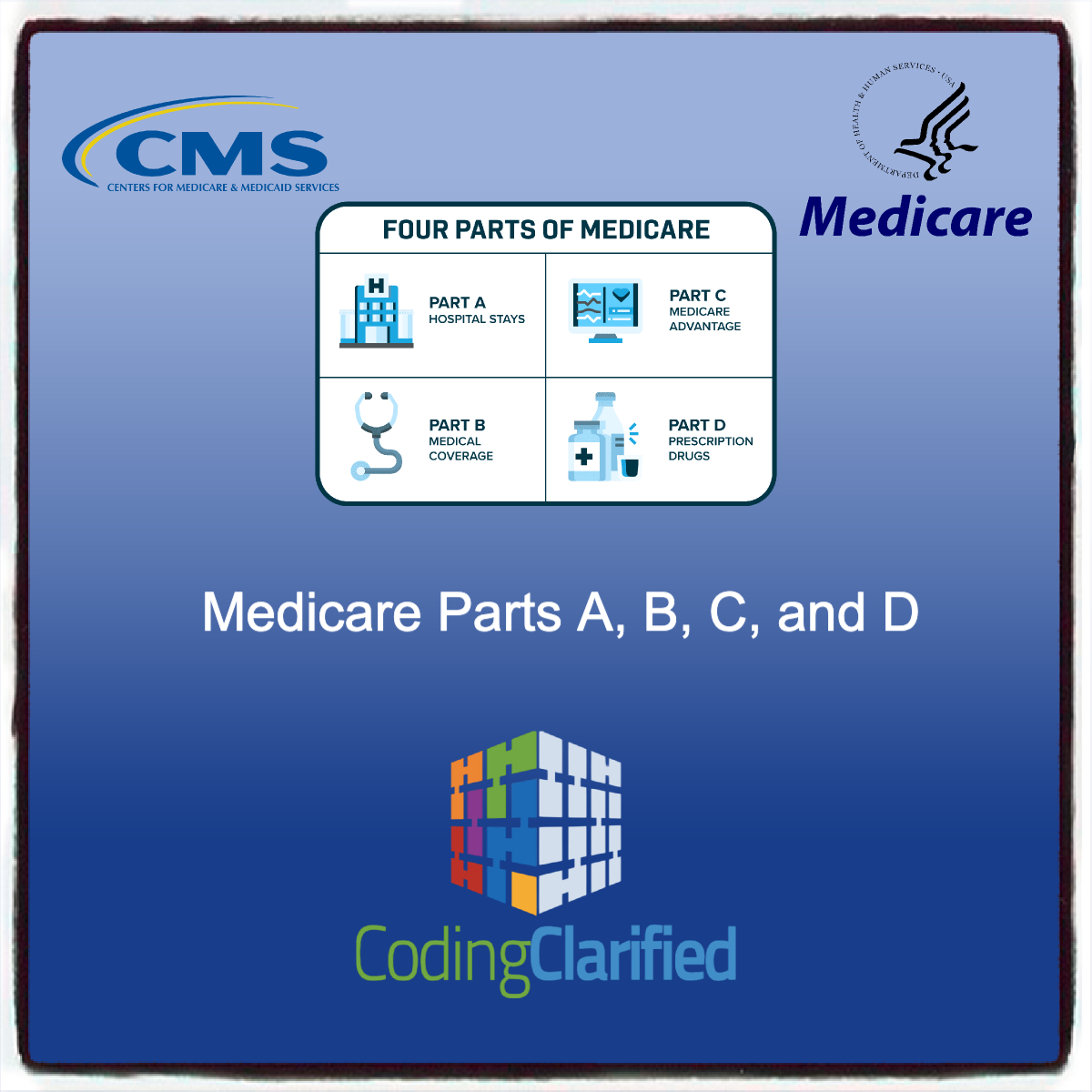
Understanding Medicare Parts A, B, C, and D: Guidelines for Medical Coding
Navigating the complexities of Medicare is crucial for medical coders to ensure accurate billing and compliance. Medicare is divided into four parts: A, B, C, and D, each serving different healthcare needs. Understanding these components and their coding guidelines is essential for healthcare providers and coders alike. This article will break down each part and its implications for medical coding.
Medicare Part A: Hospital Insurance
Overview
Medicare Part A primarily covers inpatient hospital stays, skilled nursing facility care, hospice, and some home health services.
Coding Guidelines
- Inpatient Admissions: When coding for inpatient services, coders must ensure that the appropriate ICD-10-CM diagnosis codes are used, along with the corresponding CPT/HCPCS codes for procedures.
- Length of Stay: Documentation must support the medical necessity for the length of stay, as longer stays may trigger additional scrutiny.
- DRG System: Part A uses the Diagnosis-Related Group (DRG) system for payment. Coders need to be familiar with how DRGs are assigned based on the principal diagnosis and procedures performed. https://www.utmb.edu/rco/Employees/DCDA
Medicare Part B: Medical Insurance
Overview
Part B covers outpatient services, including physician visits, preventive services, and durable medical equipment.
Coding Guidelines
- Evaluation and Management (E/M) Services: Coders should be proficient in using the correct E/M codes based on the level of service provided. Documentation must support the complexity of the visit. https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf
- Modifiers: When applicable, modifiers (e.g., 25, 59) must be used to indicate that a procedure or service was distinct or separate from other services performed on the same day. CPT Medical Modifiers https://codingclarified.com/cpt-medical-modifiers/
- Preventive Services: Coding for preventive services requires specific CPT codes, and documentation must demonstrate that services were performed according to Medicare guidelines.
Medicare Part C: Medicare Advantage Plans
Overview
Medicare Part C, or Medicare Advantage, combines the benefits of Parts A and B and may include additional benefits such as vision and dental coverage.
Coding Guidelines
- Network Restrictions: Coders must be aware of network restrictions and ensure that claims are submitted correctly based on the provider’s participation in the Medicare Advantage plan.
- Comprehensive Coding: Because Part C plans may cover additional services, coders need to accurately code for these services, following the guidelines of both Medicare and the specific Advantage plan.
- Utilization Review: Claims submitted under Part C may be subject to stricter utilization review processes. Coders must ensure that documentation justifies the medical necessity of all services rendered.
Medicare Part D: Prescription Drug Coverage
Overview
Part D provides coverage for prescription medications, allowing beneficiaries to enroll in private plans that offer drug coverage.
Coding Guidelines
- Drug Coding: While medical coders typically focus on medical services rather than pharmaceuticals, they must understand the coding for medications when they interact with healthcare services.
- NDC Codes: Coders should be familiar with National Drug Codes (NDC) when applicable, as some services may require these codes to ensure proper billing for medications.
- Documentation Requirements: Proper documentation is essential for justifying the need for specific medications, particularly if prior authorization is required.
Understanding the guidelines associated with Medicare Parts A, B, C, and D is vital for effective medical coding. Each part has distinct coverage and coding requirements that coders must navigate to ensure accurate billing and compliance. Staying updated with the latest Medicare regulations and coding standards will not only enhance the efficiency of the coding process but also contribute to improved patient care and organizational revenue. By mastering these components, medical coders can better support healthcare providers in delivering high-quality services to Medicare beneficiaries.