What is the difference between Telemedicine and Telehealth?
Telemedicine is the practice of medicine using technology to deliver care at a distance. It occurs using telecommunications between a patient (at an originating site) and a physician or other practitioner licensed to practice medicine (at a distant hub or site).
Telehealth is the use of telecommunications and information technology to provide access to health assessment, diagnosis, intervention, consultation, supervision, and information across distances. It seeks to improve a patient’s health by permitting two-way, real-time interactive communication between the patient and the physician or practitioner at a distant site.
As of 2025, medical coding guidelines for telehealth are expected to continue evolving alongside regulatory changes and technological advancements. Here are some general guidelines and trends you might anticipate based on current practices:
- CPT Codes: Familiarize yourself with the latest Current Procedural Terminology (CPT) codes specifically designated for telehealth services. Codes for virtual visits, remote patient monitoring, and other telehealth-related services may be updated.
- Modifiers: Use the appropriate modifiers, such as 95 for telehealth services provided via real-time audio and video technology. Ensure you stay updated on any new modifiers introduced.
- Documentation Requirements: Thorough documentation is essential. Providers must document the modality of the visit (e.g., audio, video), patient consent, and the specific services rendered during the telehealth encounter.
- Patient Location: Be aware of the rules regarding the patient’s location during the telehealth visit. Some payers require the patient to be in specific locations (e.g., at home, in a healthcare facility) to qualify for reimbursement.
- Coverage Variations: Different insurers may have varying coverage for telehealth services. Ensure you are familiar with the specific policies of Medicare, Medicaid, and private payers.
- New Codes for Remote Monitoring: As remote patient monitoring continues to grow, look for updates in coding guidelines that may introduce new codes for remote services, including chronic care management and patient engagement tools.
- Interstate Licensure: Be aware of the implications of interstate licensure for telehealth services, especially if coding involves care provided across state lines. This may impact reimbursement eligibility.
- Compliance with HIPAA: Ensure that all telehealth practices comply with HIPAA regulations for patient privacy and data security. This is crucial for maintaining trust and ensuring proper coding.
- Continuing Education: Stay updated through webinars, coding workshops, and guidelines from organizations like the American Academy of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA).
- Feedback Loop: Engage in regular reviews of coding practices and feedback from claims submissions to adapt to ongoing changes and improve accuracy.
In the Evaluation and Management (E/M) section, there are 17 new telemedicine codes (98000-98016), effective Jan. 1, 2025
CPT 2025 will include new codes for audio-only telemedicine visits for new patients (98008-98011) and established patients (98012-98015). These expanded codes will replace the existing telephone-only codes 99441-99443, which CPT 2025 will delete.
New telemedicine code debuting in 2025, 98016 (Brief communication technology-based service (eg, virtual check-in) by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related evaluation and management service provided within the previous 7 days nor leading to an evaluation and management service or procedure within the next 24 hours or soonest available appointment, 5-10 minutes of medical discussion). It will replace the existing HCPCS code G2012.
Here are some CPT codes for telehealth services in 2025:
- 9X091: A new code for a brief virtual check-in encounter
- 98975: Updated to include digital therapeutic intervention
- 98976-98978: Revised to include device supply for data access or data transmissions
Other telehealth-related changes in 2025 include:
- CMS will suspend frequency limitations for subsequent inpatient visits, subsequent nursing facility visits, and critical care consultation services
- CMS will keep looser direct supervision requirements for audio-visual telehealth services in certain circumstances
- Providers who perform telehealth services from home can continue to report services under their office address
- Statutory restrictions on location, site of service, and practitioner type will go back into effect
CPT New patients:
-
98000 – Synchronous audio-video visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision-making. When using total time on the date of the encounter for code selection, 15 minutes must be met or exceeded
-
98001 – …which requires a medically appropriate history and/or examination and low medical decision-making. When using total time on the date of the encounter for code selection, 30 minutes must be met or exceeded
-
98002 – …which requires a medically appropriate history and/or examination and moderate medical decision-making. When using total time on the date of the encounter for code selection, 45 minutes must be met or exceeded
-
98003 – which requires a medically appropriate history and/or examination and high medical decision-making. When using total time on the date of the encounter for code selection, 60 minutes must be met or exceeded
CPT Established patients:
-
98004 – Synchronous audio-video visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and straightforward medical decision-making. When using total time on the date of the encounter for code selection, 10 minutes must be met or exceeded.
-
98005 – … which requires a medically appropriate history and/or examination and low medical decision-making. When using total time on the date of the encounter for code selection, 20 minutes must be met or exceeded
-
98006 – …which requires a medically appropriate history and/or examination and moderate medical decision-making. When using total time on the date of the encounter for code selection, 30 minutes must be met or exceeded
-
98007 – … which requires a medically appropriate history and/or examination and high medical decision-making. When using total time on the date of the encounter for code selection, 40 minutes must be met or exceeded.
Before the PHE, the following frequency limitations were in place:
- Limit of one telehealth visit every three days for subsequent inpatient visits;
- Limit of one telehealth visit every 14 days for subsequent nursing facility visits; and
- Limit on critical care consultations to one telehealth visit per day.
CMS proposed to continue to delay through December 31, 2025, before reinstating limitations on the number of times certain services in high-acuity settings may be performed via telehealth. During this time, CMS will continue to evaluate whether the removal of these frequency limitations should be made permanent.
The extension of CMS’s current suspension of frequency limitations applies to the following codes:
- Subsequent inpatient visit CPT codes 99231, 99232, 99233;
- Subsequent nursing facility visit CPT codes 99307, 99308, 99309, 99310; and
- Critical Care Consultation Services HCPCS codes G0508, G0509.
Telehealth Services under the PFS
For CY 2025, CMS proposed to add several services to the Medicare Telehealth Services List on a provisional basis, including demonstration prior to initiation of home International Normalized Ratio (INR) monitoring and caregiver training services. They were proposing to continue the suspension of frequency limitations for subsequent inpatient visits, subsequent nursing facility visits, and critical care consultations for CY 2025. https://www.cms.gov/medicare/coverage/telehealth/list-services
CMS proposed that beginning January 1, 2025, an interactive telecommunications system may include two-way, real-time audio-only communication technology for any telehealth service furnished to a beneficiary in their home if the distant site physician or practitioner is technically capable of using an interactive telecommunications system but the patient is not capable of, or does not consent to, the use of video technology.
CMS proposed that, through CY 2025, we will continue to permit the distant site practitioner to use their currently enrolled practice location instead of their home address when providing telehealth services from their home.
CMS proposed, for a certain subset of services that are required to be furnished under the direct supervision of a physician or other supervising practitioner, to permanently adopt a definition of direct supervision that allows the physician or supervising practitioner to provide such supervision through real-time audio and visual interactive telecommunications. CMS specifically proposed that the physician or supervising practitioner may provide such virtual direct supervision for services furnished incident to a physician’s service when they are provided by auxiliary personnel employed by the physician and working under his or her direct supervision and for which the underlying HCPCS code has been assigned a PC/TC indicator of office or other outpatient visit for the evaluation and management of an established patient who may not require the presence of a physician or other qualified health care professional. For all other services furnished under the direct supervision of the supervising physician or other practitioner, we are proposing to continue to define “immediate availability” to include real-time audio and visual interactive telecommunications technology only through December 31, 2025.
CMS proposed to continue our current policy to allow teaching physicians to have a virtual presence for purposes of billing for services furnished involving residents in all teaching settings, but only in clinical instances when the service is furnished virtually (for example, a three-way telehealth visit, with the patient, resident, and teaching physician all parties in separate locations) through December 31, 2025. This virtual presence will continue to meet the requirement that the teaching physician be present for the key portion of the service. We are also requesting information to help us consider whether and how best to expand the array of services included under the primary care exception in future rulemaking.
CMS transformed the working definition of “direct supervision” over the course of the public health emergency. The definition was updated in regard to supervision for the following:
- Diagnostic tests
- Physician’s services
- And certain hospital outpatient services
The 2025 Medicare Physician Fee Schedule (MPFS) includes several changes, including:
-
Conversion factor
The conversion factor for 2025 is proposed to be $32.36, a 2.8% decrease from 2024. This is due to the expiration of the 2.93% increase for 2024, as well as a small budget neutrality adjustment.
-
G2211 complexity add-on code
This code can be paid when the base code is reported on the same day as a preventive service, such as a vaccine administration or annual wellness visit. For CY 2025, CMS proposed to allow payment of the O/O E/M visit complexity add-on code G2211 when the O/O E/M base code is reported by the same practitioner on the same day as an annual wellness visit (AWV), vaccine administration, or any Medicare Part B preventive service furnished in the office or outpatient setting.
-
Telehealth flexibilities
Several telehealth flexibilities implemented during the COVID-19 pandemic will be maintained or extended.
-
Digital mental health treatment
Three new G codes will be established for reporting digital mental health treatment.
-
MIPS performance thresholds
MIPS performance thresholds will be revised.
-
Infectious disease physician services
A new add-on code, HCPCS code GIDXX, was created to describe the intensity and complexity of hospital inpatient or observation care for infectious diseases.
-
Preventive vaccines in RHCs and FQHCs
RHCs and FQHCs will be allowed to bill for Part B preventive vaccines and their administration at the time of service.
-
Direct supervisionDirect supervision will be permitted through real-time audio and visual interactive telecommunications until December 31, 2025.
New Additions to the List of Telehealth Services:
CMS proposed adding certain codes to the Proposed List of Telehealth Services on a provisional basis. The List includes the services that are payable under the Medicare Physician Fee Schedule when furnished via telehealth. No codes are proposed to be added on a permanent basis, but the proposed provisional additions include:
- HCPS Code G0248 (Home International Normalized Ratio Monitoring)
- HCPS Code G0011 (PrEP for HIV)
- HCPS Code G0013 (PrEP for HIV)
- HCPS Codes GCTD1 – 3 (Caregiver Training In Direct Care Strategies and Techniques)
- HCPS Codes GCTB1 – 2 (Individual Behavior Management/Modification Caregiver Training)
- CPT Codes 97550-97552 (Caregiver Training in Strategies To Facilitate Patient Functional Performance in the Home or Community)
- CPT Codes 96202 – 96203 (Group Behavior Management/Modification Caregiver Training)
No Recognition of New AMA Telemedicine Evaluation and Management (E/M) Services Codes
For 2025, the most significant medical coding update for telemedicine services is the introduction of 17 new CPT codes (98000-98016) specifically for telemedicine visits including separate codes for audio-video and audio-only encounters for both new and established patients, effectively replacing the old telephone-only codes (99441-99443) which are being deleted; additionally, a new code (98016) will be used for brief virtual check-in encounters replacing the HCPCS code G2012.
-
New codes for different telemedicine types:
New codes will be used for audio-video telemedicine visits for new and established patients (98000-98007) and separate codes for audio-only visits (98008-98015).
-
Deletion of old telephone codes:
The existing telephone-only codes (99441-99443) will be removed from the CPT code set.
-
Virtual check-in code:
A new code (98016) will be used for brief virtual check-in encounters.
-
No significant changes to telehealth eligibility:While new codes are being implemented, the overall eligibility criteria for telehealth services is expected to remain largely the same
The American Medical Association (“AMA”) recently revised the CPT Codebook and valued seventeen new codes (9X075 – 9X091) to describe telemedicine Evaluation and Management (“E/M”) services. CMS proposes to decline recognizing and paying for the new codes because they mirror existing office/outpatient E/M codes. For those new codes, CMS also proposes assigning a procedure status indicator of “I” to indicate that there is a more specific code that should be used for Medicare purposes.
Always consult official sources or coding specialists for the most accurate and updated information as guidelines can change frequently.
HCPCS code Q3014
-
What it is:Q3014 is specifically for the facility where the patient is located during a telehealth visit, not the provider’s location.
-
When to use it:The facility where the patient is located during the telehealth visit can bill Q3014, as long as the facility is an eligible originating site.
-
Eligible Originating Sites:These include physician or practitioner offices, hospitals, critical access hospitals, rural health clinics, federally qualified health centers, community mental health centers, skilled nursing facilities, and hospital-based or CAH-based renal dialysis centers.
-
Payment:Medicare reimburses the originating site facility fee for these services, as described by HCPCS Q3014.
-
Distant Site Provider:The distant site provider (the provider providing the telehealth service) bills separately for their professional services.
-
No Modifier 95:Modifier 95 is not used with Q3014.
-
Telehealth Services:Q3014 is used for telehealth services rendered via interactive audio and video telecommunications systems.
-
Place of Service (POS):For professional claims, use the POS that represents the location from which the telemedicine visit was rendered.
-
Documentation:Providers must document the provider and patient location (city/town, state, ZIP code) in the medical record.
-
Payment Amount:The payment amount for Q3014 is 80% of the lesser of the actual charge ($29.96 for CY 2024 services and $31.04 for CY 2025 services).
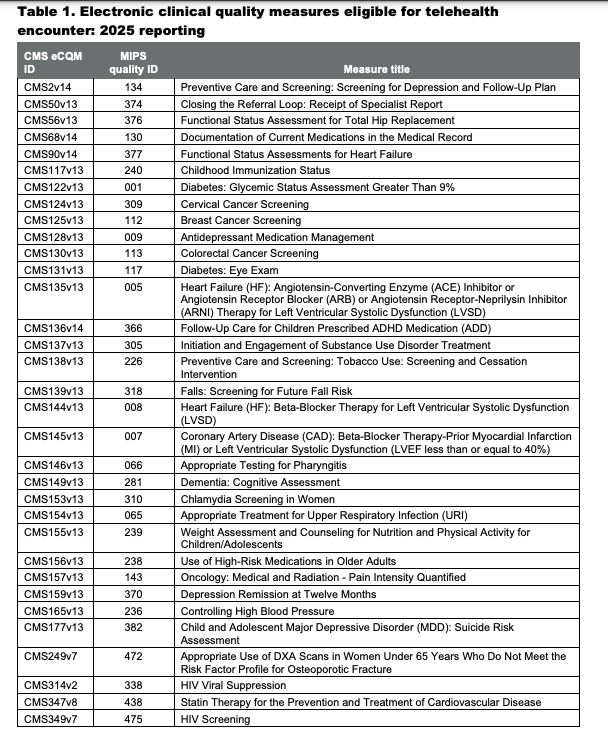
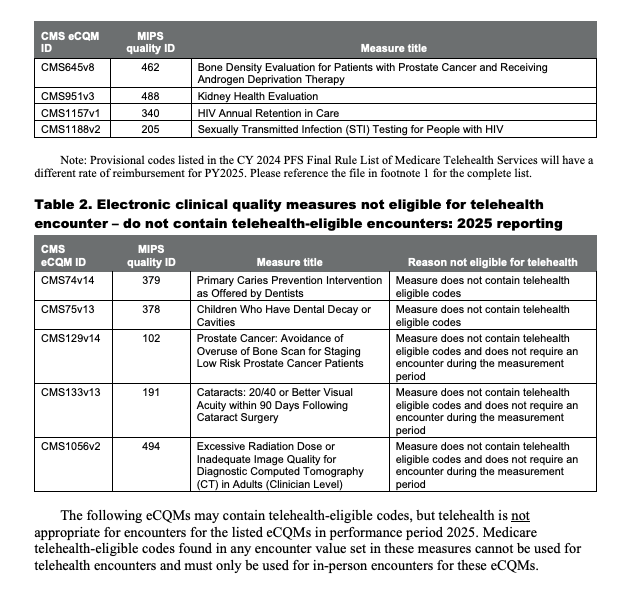
https://ecqi.healthit.gov/sites/default/files/2025-EC-Telehealth-Guidance.pdf
Let Coding Clarified “Clarify” coding for you:
Read our daily blog:
https://codingclarified.com/medical-coding-blog/
Follow Coding Clarified on FaceBook:
https://www.facebook.com/codingclarified/

