Medical Coding for Dehydration Guidelines
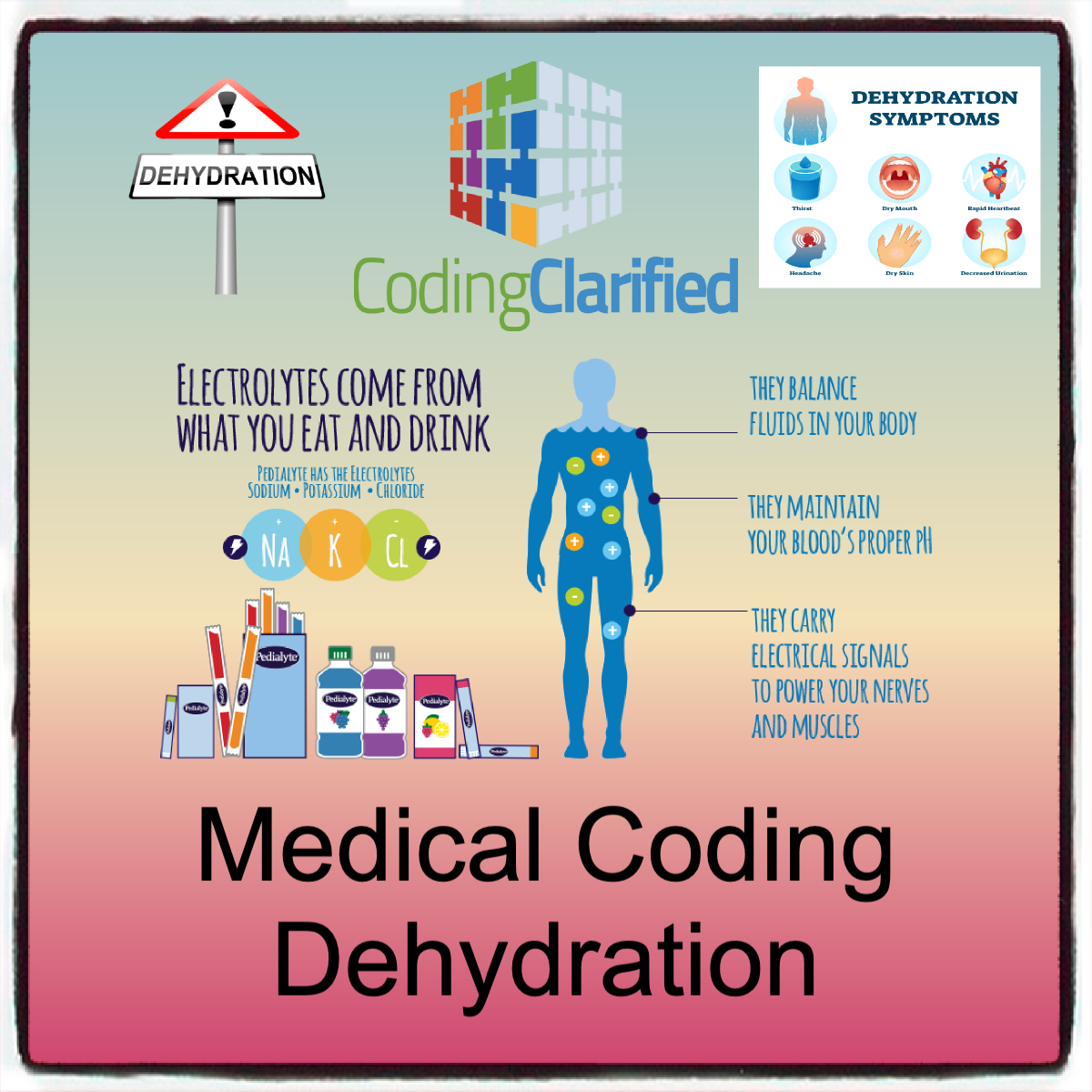
Dehydration is a common condition that occurs when the body loses more fluids than it takes in, leading to an imbalance of electrolytes and fluids essential for normal bodily functions. While dehydration can range from mild to severe, it often requires medical attention, especially when it’s caused by factors like illness, fever, vomiting, diarrhea, or excessive sweating. The proper medical coding for dehydration-related services are essential for healthcare providers to receive appropriate reimbursement and maintain compliance with payer requirements.
This blog will outline the key guidelines for medical coding and billing for dehydration, focusing on the diagnostic codes, procedures for treatment (like IV hydration), and important documentation practices to ensure accurate claims.
ICD-10-CM Codes for Dehydration
The first step in coding for dehydration is to assign the correct ICD-10-CM diagnosis code. The ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) provides specific codes to identify different types and causes of dehydration, including the severity and the underlying cause.
Common ICD-10 Codes for Dehydration
- E86.0: Dehydration
- This is the most general code used for dehydration without specifying the underlying cause. It is appropriate when the cause of dehydration is not specified or is non-acute.
- E86.1: Hypovolemia
- Used when dehydration is associated with a decrease in blood volume due to fluid loss.
- E86.2: Dehydration due to Diarrhea
- This code is used when dehydration is specifically caused by diarrhea, a common cause of fluid loss.
- E86.3: Dehydration due to Vomiting
- This code applies when vomiting leads to dehydration.
- E86.4: Dehydration due to Excessive Sweating
- This code is appropriate for dehydration caused by excessive sweating, such as in cases of heatstroke or heavy physical activity.
- E86.8: Other Dehydration
- This code is used for dehydration due to causes not specifically listed in the other categories, such as excessive urination or inadequate intake.
- E86.9: Dehydration, Unspecified
- This code is used when dehydration is diagnosed, but the specific cause is not clear or not documented.
Severity of Dehydration
It’s important to note that dehydration can vary in severity, ranging from mild to severe. While the ICD-10 codes above primarily focus on dehydration as a condition, healthcare providers should consider specifying the severity of dehydration when appropriate. Severity levels may influence treatment and billing practices. Severe dehydration may require more intensive intervention, such as hospitalization and IV fluid replacement.
CPT Codes for Dehydration Treatment
Once the diagnosis code is established, the next step is to code for the treatment provided to address the dehydration. The most common treatment for dehydration, especially in more severe cases, is intravenous (IV) hydration, which involves the administration of fluids directly into a patient’s bloodstream to restore hydration and electrolytes.
The CPT (Current Procedural Terminology) codes used to report IV hydration services fall under the “Injection and Infusion” section of the CPT manual.
Common CPT Codes for IV Hydration and Dehydration Treatment
- 96360: Hydration, Intravenous Infusion, Initial
- This code is used when the patient receives an intravenous infusion for hydration. The first hour of the infusion is billed under this code.
- 96361: Hydration, Intravenous Infusion, Each Additional Hour
- This code is used when the hydration treatment continues for more than one hour, and each additional hour of infusion is billed separately.
- 96365: IV Infusion of Medication, Initial Hour
- This code can be used for the infusion of other medications besides fluids, such as electrolyte replenishment or medications given as part of the dehydration treatment plan (for example, potassium or sodium bicarbonate).
- 96366: IV Infusion of Medication, Each Additional Hour
- This code is used for each additional hour of medication infusion.
- 96374: Therapeutic, Prophylactic, or Diagnostic Injection
- Used to report injections (such as anti-nausea medications or electrolytes) given in conjunction with hydration therapy.
- 96375: Injection, Hydration (IV)
- A code used for the administration of hydration therapy, especially in outpatient or emergency settings.
Other Hydration-Related Procedures
- CPT Code 36415: Collection of Venous Blood by Venipuncture
- Often used to monitor fluid levels, electrolytes, and kidney function in patients receiving hydration treatment. This code would be applicable if bloodwork is performed as part of the dehydration assessment.
- CPT Code 96372: Injection, Subcutaneous or Intramuscular
- This code can be used for subcutaneous or intramuscular fluid administration in cases where IV hydration is not required, although this is less common for dehydration.
Key Considerations for Accurate Billing
Documentation
Accurate and thorough documentation is essential for coding dehydration and its treatment. The documentation should clearly indicate:
- The cause of dehydration (e.g., diarrhea, vomiting, excessive sweating).
- The severity of dehydration (e.g., mild, moderate, severe).
- The type of treatment provided (e.g., IV hydration, oral rehydration therapy).
- The duration of the treatment (e.g., how long the IV infusion lasted, whether the treatment was extended).
- The outcome of the treatment (e.g., improvement in hydration status, vital signs returned to normal).
The more detailed and precise the documentation, the more likely the claim will be reimbursed without issues.
Modifier Use
In some cases, modifiers may be required to further clarify the services provided:
- Modifier 25: Used when a significant and separately identifiable evaluation and management (E/M) service is provided on the same day as the hydration treatment. For example, if a physician performs an assessment for dehydration (E/M) and administers hydration therapy during the same visit.
- Modifier 59: Used to indicate that a procedure (e.g., hydration) is distinct or separate from another procedure (e.g., an unrelated diagnostic test or another treatment).
CPT Modifiers https://codingclarified.com/cpt-medical-modifiers/
Level of Care
The level of care in which the dehydration treatment is provided impacts the coding and billing process:
- Outpatient Care: Dehydration treatment in an outpatient setting (e.g., urgent care or physician’s office) is typically billed with the appropriate CPT codes for IV hydration and any associated medications.
- Emergency Department (ED): Dehydration in the ED may require additional E/M codes and possibly higher levels of billing, depending on the severity of the dehydration and any additional services provided.
- Inpatient Care: If the dehydration is severe enough to require hospitalization, different inpatient coding rules apply. Hospital charges would include codes for both hydration treatment and any related procedures (such as blood tests, imaging, or additional medications).
Bundling and Separate Billing
In some cases, certain dehydration-related treatments or tests might be bundled into a single code. For example, a basic hydration infusion may include monitoring and follow-up care. However, if additional services (like lab work or specialized treatments) are performed, they may need to be billed separately. Coders should be familiar with bundling rules to ensure services are billed correctly and to avoid overbilling or underbilling.
Medical Coding Bundling and Upcoding Guidelines https://codingclarified.com/medical-coding-bundling-and-upcoding-guidelines/
Challenges in Medical Coding for Dehydration
- Under-documentation: Dehydration can be difficult to diagnose in some cases, particularly when patients present with vague symptoms or when dehydration is secondary to another underlying condition. Ensuring thorough documentation is vital to justify the treatment and services provided.
- Overlapping Services: Dehydration is often a secondary diagnosis, with other conditions (e.g., infection, electrolyte imbalance) requiring treatment. Coders must differentiate between the primary condition and the dehydration treatment to avoid confusing claims.
- Hydration as a Symptom or Standalone Condition: In some instances, hydration is provided as part of the treatment for another condition (e.g., dehydration due to an infection). Understanding the full context of the treatment can help ensure the correct codes are used.
Accurate coding and billing for dehydration treatment are essential for healthcare providers to receive appropriate reimbursement and avoid claim denials. By understanding the correct ICD-10-CM diagnosis codes for dehydration, the CPT codes for hydration and related treatments, and the importance of thorough documentation, providers can ensure that they comply with coding standards and payer requirements. Regular training and staying updated on coding guidelines will help ensure that hydration treatments for dehydration are coded and billed correctly for optimal reimbursement
CMS Billing and Coding: Hydration Services https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=52732&ver=24&articleStatus=all&sortBy=title&bc=3