Medical Coding and Billing Guidelines for Cardiology: STEMI and NSTEMI
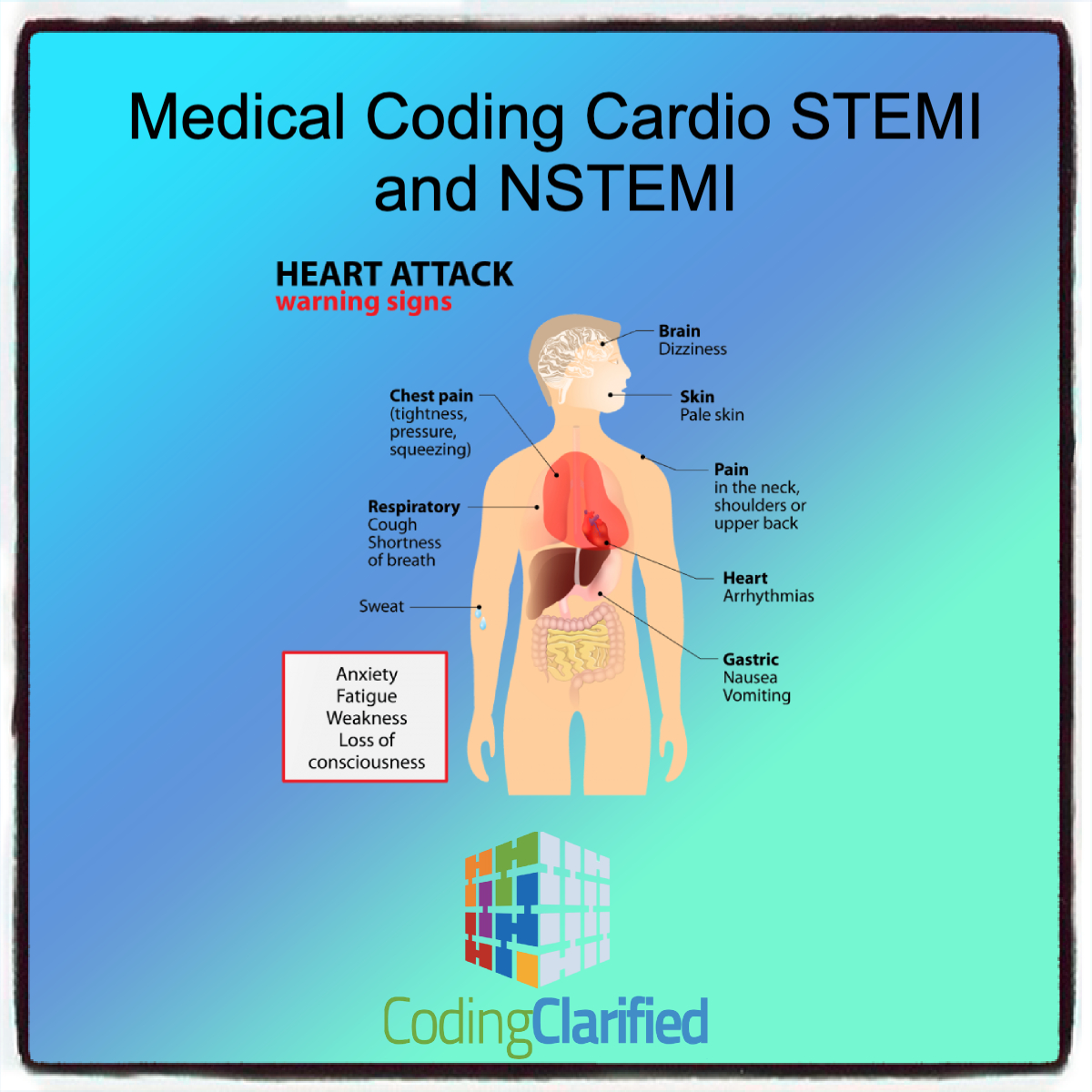
STEMI (ST-Elevation Myocardial Infarction) and NSTEMI (Non-ST-Elevation Myocardial Infarction) are two distinct types of heart attacks, each requiring specific diagnostic and procedural coding. Accurate coding and billing are essential for ensuring proper reimbursement, compliance, and patient care tracking. Below are the key guidelines for coding and billing STEMI and NSTEMI, focusing on the ICD-10-CM (diagnostic) codes, CPT (procedural) codes, and relevant documentation requirements.
1. ICD-10-CM Codes for STEMI and NSTEMI
ICD-10-CM (International Classification of Diseases, 10th Edition, Clinical Modification) codes are used to classify and code diagnoses. For myocardial infarction, the following classifications apply:
STEMI (ST-Elevation Myocardial Infarction) Codes
STEMI is typically diagnosed when there is an elevation of the ST segment on an electrocardiogram (ECG) alongside myocardial injury. It involves the complete or near-complete blockage of a coronary artery.
- I21.0 – I21.9: Acute Myocardial Infarction (MI) codes, depending on the location and other factors.
- I21.0: Anterior wall STEMI
- I21.1: Inferior wall STEMI
- I21.9: Acute MI, unspecified (use only when exact location is unknown)
NSTEMI (Non-ST-Elevation Myocardial Infarction) Codes
NSTEMI involves less severe damage to the heart muscle compared to STEMI and is typically diagnosed when there are elevated biomarkers (troponin levels) but no significant ST-segment elevation.
- I21.4 – I21.9: These codes also cover NSTEMI based on the affected area and other clinical details.
- I21.4: Non-ST elevation (NSTEMI), subendocardial
- I21.9: Unspecified acute myocardial infarction (may be used if the type of infarction is unclear)
Documentation for Accurate Coding
To assign the correct ICD-10-CM code, it is important that the physician’s documentation clearly specifies:
- The type of myocardial infarction (STEMI or NSTEMI)
- The location of the infarction (anterior, inferior, lateral, etc.)
- Any complications or co-existing conditions
- The exact timing of the infarction (acute, subacute, etc.)
2. CPT Codes for Procedures Related to STEMI and NSTEMI
CPT (Current Procedural Terminology) codes are used to report procedures and services. In the context of STEMI and NSTEMI, the following procedural codes may apply:
Cardiac Catheterization and PCI (Percutaneous Coronary Intervention)
- CPT Code 93452: Diagnostic catheterization of coronary arteries (left and right heart catheterization).
- CPT Code 92920: Percutaneous transluminal coronary angioplasty (PTCA) for the treatment of coronary artery disease (CAD).
- CPT Code 92941: Percutaneous coronary intervention (PCI), including stent placement (if applicable).
- CPT Code 92928: Coronary artery stent placement, one or more coronary arteries. https://codingclarified.com/medical-coding-cardiac-catheterization/
Thrombolytic Therapy
For STEMI cases where thrombolytic therapy is administered:
- CPT Code 92973: Thrombolytic therapy for myocardial infarction.
Other Related Services
- CPT Code 93000: Electrocardiogram (ECG) – typically for STEMI diagnosis.
- CPT Code 92929: Atherectomy, coronary, with PCI, if performed as part of the STEMI or NSTEMI treatment.
Documentation for Procedures
Accurate coding for these procedures requires detailed documentation of:
- The type of procedure performed (e.g., angioplasty, stent placement, thrombolysis).
- The specific coronary artery treated.
- Any complications or adverse events during the procedure.
- The use of any adjunctive therapies, such as antiplatelet agents or anticoagulants.
3. Modifiers and Billing
Modifiers are used to provide additional information about a procedure or service, such as whether a service was altered in some way. In cardiology, the following modifiers might be relevant:
- Modifier 59: Distinct procedural service (used when procedures performed are not part of a bundled code).
- Modifier 24: Unrelated evaluation and management service by the same physician during a postoperative period (e.g., when a patient presents for additional care during hospitalization for STEMI/NSTEMI). https://codingclarified.com/cpt-medical-modifiers/
Billing for Multiple Procedures
If multiple procedures are performed during the same visit (e.g., cardiac catheterization and PCI), it’s important to follow correct billing guidelines. Bundle payment rules may apply, and separate line items should be billed for each distinct service.
4. ICD-10-PCS Codes (Inpatient Settings)
If the patient is hospitalized and undergoes surgery or invasive procedures related to STEMI or NSTEMI, ICD-10-PCS (Procedure Coding System) codes will be used in inpatient settings:
- 027034Z: Percutaneous coronary intervention (PCI) to treat the coronary artery for myocardial infarction.
- 0270XX0: Insertion of stent, coronary artery.
ICD-10-PCS codes require accurate documentation of the procedure, approach (e.g., percutaneous or open), and device used.
5. Considerations for Comorbidities and Complications
Cardiologists should also consider the presence of comorbid conditions when coding and billing for STEMI or NSTEMI. Conditions like hypertension, diabetes, or congestive heart failure that may impact the treatment plan should be documented and coded appropriately using additional ICD-10-CM codes.
- I10 – I15: Hypertension codes
- E11 – E14: Diabetes codes
- I50.1: Left ventricular heart failure
These conditions might impact the patient’s treatment protocol and may influence reimbursement rates.
6. Avoiding Common Coding Errors
- Misdiagnosis of STEMI vs. NSTEMI: Ensure clear differentiation between STEMI and NSTEMI based on diagnostic tests (e.g., ECG findings, troponin levels).
- Incomplete documentation: Accurate, thorough documentation of clinical findings and procedures is critical for accurate coding.
- Incorrect use of unspecified codes: Avoid using unspecified codes like I21.9 unless absolutely necessary, as they can lead to claim denials or delays.
- Underreporting of comorbid conditions: Failing to report relevant comorbidities can affect the completeness of the coding and impact reimbursement.
Accurate coding and billing for STEMI and NSTEMI require careful attention to clinical details and procedure documentation. Providers must use appropriate ICD-10-CM, CPT, and ICD-10-PCS codes, apply modifiers where necessary, and ensure that the patient’s full clinical picture, including comorbid conditions, is reflected in the coding process. Proper coding not only ensures compliance but also supports appropriate reimbursement for cardiology services related to heart attacks.
The key features to diagnose a type 2 MI are as follows:
● An elevated but changing troponin value
● Clinical features inconsistent with type 1 acute MI
● Clinical conditions known to increase the oxygen demand or decrease the
oxygen supply like tachycardia
● Potentially confounding clinical conditions or comorbidities that are
potentially associated or known to be associated with myocardial injury
● Symptoms of acute myocardial ischemia such as typical chest pain.
● New ischemic ECG changes.
● Development of pathological Q waves.
● Imaging evidence of new loss of viable myocardium, significant reversible
perfusion defect on nuclear imaging, or new regional wall motion abnormality
in a pattern consistent with an ischemic etiology.
● Absence of symptoms and/or signs indicating other nonischemic causes of
troponin elevations like myocarditis.
Treatment of type 2 MI is to treat the underlying condition. To adequately assess the
prognosis and determine appropriate further treatment in patients with type 2 MI,
information about whether the patient has (or is likely to have) significant underlying CAD
is essential.
A TYPE 2 MI WILL NEVER BE THE PRINCIPAL DIAGNOSIS
Acute myocardial infarction (AMI)
Type 1 ST elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI) The ICD-10-CM codes for type 1 acute myocardial infarction (AMI) identify the site, such as anterolateral wall or true posterior wall. Subcategories I21.0-I21.2 and code I21.3 are used for type 1 ST elevation myocardial infarction (STEMI). Code I21.4, Non-ST elevation (NSTEMI) myocardial infarction, is used for type 1 non-ST elevation myocardial infarction (NSTEMI) and nontransmural MIs.
If a type 1 NSTEMI evolves to STEMI, assign the STEMI code. If a type 1 STEMI converts to NSTEMI due to thrombolytic therapy, it is still coded as STEMI.
For encounters occurring while the myocardial infarction is equal to, or less than, four weeks old, including transfers to another acute setting or a postacute setting, and the myocardial infarction meets the definition for “other diagnoses” (see Section III, Reporting Additional Diagnoses), codes from category I21 may continue to be reported. For encounters after the 4 week time frame and the patient is still receiving care related to the myocardial infarction, the appropriate aftercare code should be assigned, rather than a code from category I21. For old or healed myocardial infarctions not requiring further care, code I25.2, Old myocardial infarction, may be assigned.
By adhering to these guidelines, healthcare providers can streamline the billing process, reduce claim denials, and ensure that patients receive the highest standard of care.