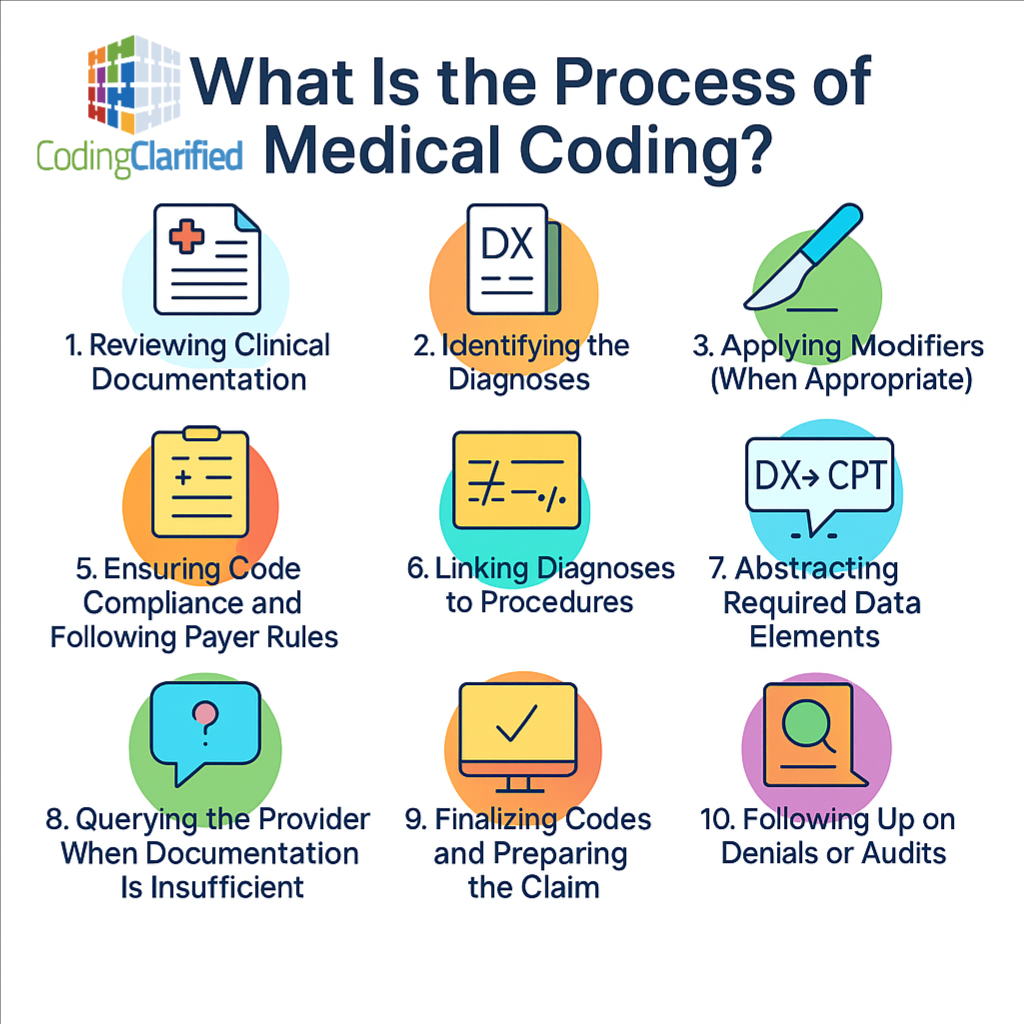
A Step-by-Step Guide for New and Experienced Coders
Medical coding is the backbone of healthcare reimbursement. It transforms the clinical story of a patient’s encounter into standardized, billable codes used for payment, reporting, data analytics, and quality tracking. But what is the process of medical coding from start to finish?
Whether you’re new to the field or strengthening your existing skills, understanding the full workflow helps you code more accurately, efficiently, and confidently. Below is a clear breakdown of the end-to-end medical coding process that happens in every healthcare setting—from clinics and hospitals to telehealth and specialty practices.
Reviewing Clinical Documentation
The first and most critical step is reviewing the provider’s documentation. Coders analyze the entire medical record for the encounter, which may include:
-
History and physical (H&P)
-
Office or progress notes
-
Operative reports
-
Diagnostic test results
-
Imaging interpretations
-
Discharge summaries
-
Telehealth documentation
-
Emergency department notes
A coder’s role is to understand what was documented, why services were performed, and what conditions were evaluated, monitored, or treated. Clear, complete documentation drives correct code selection.
Identifying the Diagnoses
Once documentation is reviewed, coders assign ICD-10-CM codes to represent:
-
The primary reason for the encounter
-
Secondary diagnoses
-
Chronic conditions affecting care
-
Complications
-
Status codes (e.g., long-term medication use, presence of devices)
-
External cause codes when required
Coders must follow ICD-10-CM Official Guidelines each step of the way—including late effects, “use additional code” notes, combination codes, and Excludes 1/2 rules. ICD-10 Steps To Code
Identifying the Procedures and Services
Next, coders determine which procedures, services, or supplies should be coded. This includes:
-
Office visits (E/M services)
-
Surgical procedures
-
Diagnostic tests
-
Lab work
-
Radiology services
-
Therapies (PT, OT, SLP)
-
Infusions/injections
-
Preventive services
-
Telehealth services
-
Supplies and durable equipment (HCPCS Level II)
From here, coders assign CPT and HCPCS codes that represent what the provider did. CPT Steps To Code
Applying Modifiers (When Appropriate)
Modifiers add essential detail that affects reimbursement. Coders determine whether modifiers are needed to clarify:
-
Laterality (RT/LT)
-
Multiple procedures
-
Repeat procedures
-
Reduced or discontinued services
-
Professional vs technical component
-
Assistant surgeon involvement
-
Telehealth modality
-
Therapy assistant involvement (CQ/CO)
-
Critical care bundling requirements
-
Global surgical package scenarios
Correct modifier use helps prevent denials and ensures accurate payment. CPT Medical Modifiers
Ensuring Code Compliance and Following Payer Rules
Medical coding is not “one size fits all.” Coders must verify:
-
NCCI (National Correct Coding Initiative) edits
-
MUE (Medically Unlikely Edits)
-
Payer-specific billing rules (Medicare, Medicaid, commercial payers)
-
LCDs/NCDs for medical necessity
-
Bundling and unbundling guidelines
-
Global surgical package requirements
-
Telehealth coverage
-
Diagnosis-to-procedure linkage for medical necessity
Compliance is key to reducing denials and protecting the organization from audits. Medical Coding Compliance
Linking Diagnoses to Procedures
The coder then links ICD-10-CM codes to the appropriate CPT/HCPCS codes to show why each service was performed.
Accurate linkage supports:
-
Medical necessity
-
Clean claims
-
Accurate reimbursement
-
Payer compliance
Incorrect linkage is one of the most common denial triggers—so coders must get this right.
Abstracting Required Data Elements
Coders extract additional data needed for billing and reporting, which may include:
-
Date of service
-
Place of service
-
Provider NPI
-
Units
-
Time-based coding elements
-
Start/stop times for infusions or E/M prolonged services
-
Surgical approach and technique
-
Device details for ICD-10-PCS
-
Anesthesia type and ASA status
This is where coding meets revenue cycle management. Abstracting from the EHR & Medical Coding OP Reports
Querying the Provider When Documentation Is Insufficient
If documentation is missing, conflicting, unclear, or incomplete, coders must send a provider query. Querying supports accuracy and compliance—not changing documentation, but clarifying it.
Common reasons for queries include:
-
Missing diagnoses
-
Laterality not documented
-
Underdocumented E/M levels
-
Conflicting data (e.g., acute vs chronic)
-
Missing surgical details
-
Clarification of complications or POA status
Coders only code what is documented, not what is assumed. Medical Coding How to Query
Finalizing Codes and Preparing the Claim
Once codes are correct and complete, they are finalized for billing. The claim is built and sent to the payer, where it will be processed for payment.
Accurate coding helps ensure:
-
Clean claims
-
Fewer denials
-
Faster reimbursement
-
Reduced audit risk
-
Correct patient billing
This is where coding directly impacts the bottom line.
Following Up on Denials or Audits
Coders may also participate in:
-
Denial management
-
Appeals
-
Audit responses
-
Education of clinical staff
-
Updating internal coding guidelines
This final step closes the loop and supports continuous improvement. Medical Coding and Billing Denials & Medical Coding Audits
Why Understanding the Coding Process Matters
Mastering the coding workflow helps coders:
-
Code with confidence
-
Avoid denials
-
Understand payer expectations
-
Strengthen critical-thinking skills
-
Communicate better with providers
-
Improve productivity
-
Protect their organization from compliance risk
Whether you’re a new coder or advancing your career, understanding the process from start to finish is essential.
Let Coding Clarified “clarify” Coding for you!
Coding Clarified can train you for the CPC, as we are an AAPC-approved education provider. You may even qualify for a scholarship/grant!
The Medical Coding course includes the following:
Access to the online medical coding course using the AAPC-approved curriculum
CPT, ICD10, HCPC, Workbook & Textbook (E-books + physical books)
1:1 time with instructor Janine as needed
Access to the Coding Clarified Collaboration
Full support and Q&A with the instructor
Instructor Janine’s audio/video files for each chapter to implement notes into your manuals
AAPC Membership
2 CPC Exam Vouchers
3 Free 50-Question bundle Practice Exams
CPC online review course
Official AAPC study guide
AAPC Practicode to remove your A (apprentice status)
Online HCC Internship to gain experience
Professional résumé assistance
career guidance /Job resources
Coding Clarified Purchase Options