Understanding the Types of Injections in Medical Coding
Injection administration is a common medical service, but proper documentation and accurate code selection are crucial for compliant billing. Let’s review the medical coding types of injections, coding guidelines, and best practices to ensure accurate reimbursement.
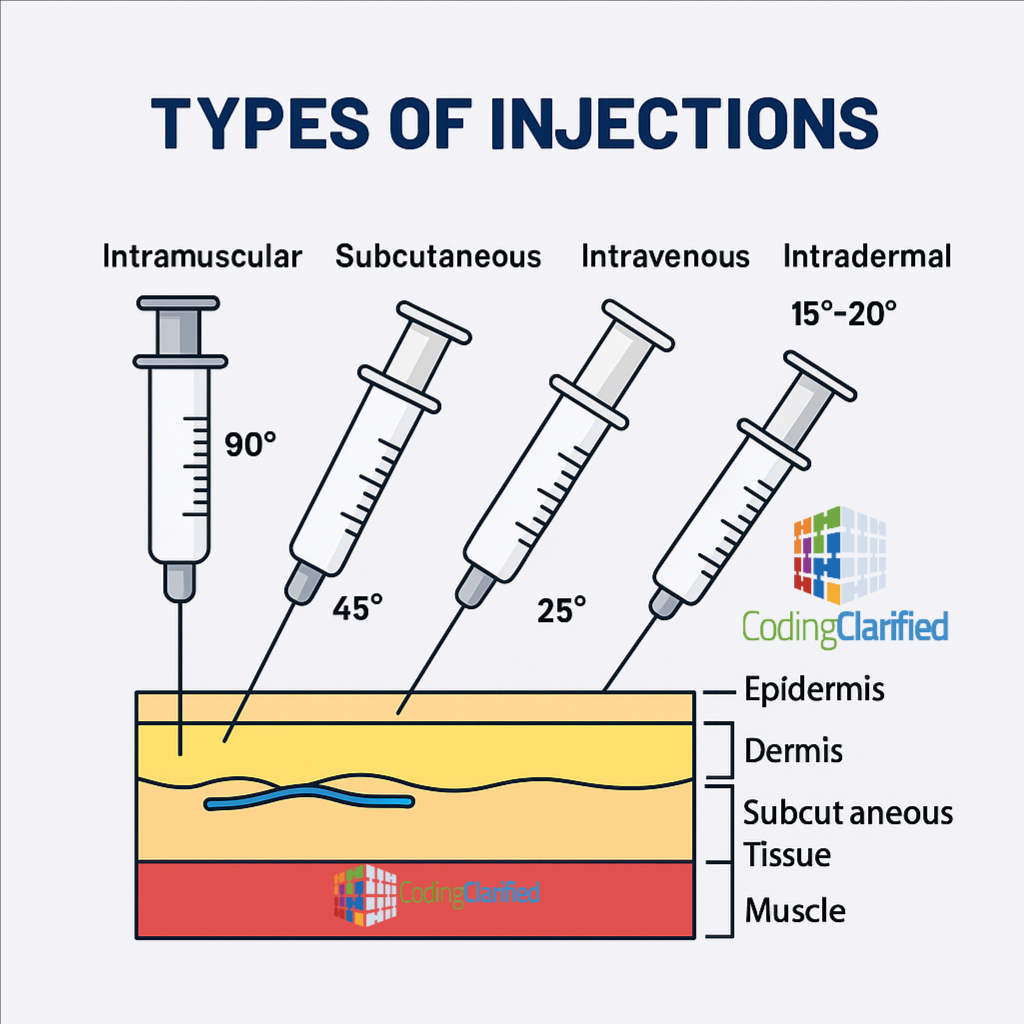
Types of Injections and Their Purposes
-
Intradermal (ID) Injections – 15° to 20°
-
Delivered into the dermis just below the skin surface.
-
Common for allergy testing or tuberculosis (TB) screening.
-
Example: Mantoux test (CPT 86580).
-
-
Subcutaneous (SC or SQ) Injections – 45°
-
Administered into the fatty tissue beneath the skin.
-
Used for slower absorption medications such as insulin or heparin.
-
Example: Insulin injection (CPT 96372 when therapeutic).
-
-
Intramuscular (IM) Injections – 90°
-
Delivered deep into muscle tissue for faster absorption.
-
Common for vaccines, antibiotics, and hormones.
-
Example: Vitamin B12 injection (CPT 96372).
-
-
Intravenous (IV) Injections – 25°
-
Administered directly into a vein for immediate effect.
-
Common for hydration therapy or medication bolus.
-
Example: IV push or infusion codes (CPT 96374–96376).
-
Injection Administration Coding (CPT 96372–96379)
CPT provides a specific range of codes for therapeutic, prophylactic, and diagnostic injections:
-
96372 – Therapeutic, prophylactic, or diagnostic injection (subcutaneous or intramuscular)
-
96373 – IV push, single or initial substance/drug
-
96374 – IV push, each additional sequential drug/substance
-
96375 – IV push, each additional sequential drug
-
96376 – IV push, same drug/substance provided more than once in the same encounter
-
96377 – Subcutaneous injection, each additional sequential injection (different medication)
💡 Note: Vaccines and toxoids are not reported with these codes; use 90460–90474 for immunization administration.
Key Documentation Requirements
Accurate documentation should include:
-
Type of injection and medication administered
-
Dosage and route (IM, SQ, ID, IV, etc.)
-
Site of administration
-
Time and date
-
Name and credentials of the provider administering the injection
-
Physician order for the injection
Incomplete documentation can lead to denials or compliance risk.
Billing and Modifier Tips
-
Include the J-code for the drug or substance (if supplied by the provider).
-
Example: J3420 for Vitamin B12 injection.
-
-
Use modifier 25 on the E/M service when both an evaluation and injection are performed on the same day, if the E/M is separately identifiable.
-
Use modifier 59 when multiple injections are performed at distinct anatomical sites.
-
Hydration therapy vs. therapeutic injection:
-
Hydration must be medically necessary and documented as the primary reason for the encounter to bill separately (CPT 96360–96361).
-
Common Denial Reasons
-
Missing or incorrect route of administration
-
Drug not documented or not linked to administration code
-
Unbundled or duplicate charges
-
Failure to apply proper modifiers when multiple injections occur
Medical Coding and Billing Denials
Coding Clarified Tips
✔ Always link the drug J-code with the administration code.
✔ Review payer policies — some carriers require NDC (National Drug Code) on claims.
✔ Ensure injections performed incident-to are properly supervised and documented.
✔ Separate immunization administration from therapeutic injections — they fall under different CPT categories.
Accurate injection coding requires careful attention to route, purpose, and documentation. Following CPT guidelines and payer requirements will help ensure full reimbursement and compliance with coding standards.
CMS Billing and Coding: Infusion, Injection and Hydration Services