Medical Coding in Nevada: An Overview of Trends, Challenges, and Opportunities
Medical coding is a crucial component of the healthcare system, translating complex medical information into standardized codes used for billing, insurance claims, and medical records. In Nevada, medical coding plays a vital role in ensuring the efficiency and accuracy of healthcare administration. This article explores the current state of medical coding in Nevada, highlighting trends, challenges, and opportunities in the field.
Current Trends in Medical Coding in Nevada
- Growing Demand for CodersThe healthcare industry in Nevada is expanding, driven by population growth, an aging demographic, and increasing healthcare needs. This expansion has led to a rising demand for skilled medical coders who can manage the complexities of medical documentation and billing. Both urban centers like Las Vegas and rural areas are seeing a need for qualified coders to support healthcare operations.
- Adoption of Advanced Coding SystemsNevada healthcare providers have fully integrated the ICD-10 coding system. It enhances the accuracy of medical records and billing processes. The ICD-10 system allows for more precise coding of diagnoses and procedures, which helps in improving patient care and reimbursement accuracy.
- Integration of Electronic Health Records (EHR)The use of EHR systems is widespread in Nevada’s healthcare facilities. These systems streamline patient data management and coding processes but also require coders to be proficient in using EHR software. The integration of EHRs helps reduce manual errors and increase efficiency, although it demands continuous learning and adaptation from medical coders.
- Focus on Compliance and AccuracyCompliance with healthcare regulations is a key concern in Nevada. With increasing scrutiny from insurance companies and regulatory bodies, there is a strong emphasis on accurate and compliant coding practices. Coders are expected to stay updated with regulatory changes and ensure that coding adheres to the latest guidelines to avoid errors and potential legal issues.
Challenges in Medical Coding in Nevada
- Shortage of Qualified CodersDespite the growing demand, Nevada faces a shortage of qualified medical coders. The specialized training and certification required for medical coding can be barriers to entry for many individuals. This shortage can lead to difficulties in finding and retaining skilled professionals, which may impact the efficiency of healthcare operations.
- Complexity of Coding SystemsThe ICD-10 coding system, while more detailed, also introduces complexity that can be challenging for coders. The need to understand a vast array of codes and keep up with frequent updates requires a high level of expertise. Coders must be adept at navigating these complexities to ensure accurate coding and billing.
- Geographic DisparitiesNevada’s vast and diverse geography presents unique challenges for medical coding. Rural and remote areas may have limited access to coding resources and training opportunities compared to urban centers. This geographic disparity can affect the availability of qualified coders and the implementation of standardized coding practices across the state.
- Data Security and PrivacyWith the increased use of digital records, ensuring data security and privacy is a significant concern. Coders must adhere to strict HIPAA (Health Insurance Portability and Accountability Act) guidelines to protect sensitive patient information. Maintaining data security while managing large volumes of information is a critical challenge for coders in Nevada.
Opportunities for Growth and Improvement
- Educational Programs and CertificationAddressing the shortage of qualified coders involves expanding educational opportunities and certification programs in Nevada. Community colleges and online institutions offer specialized programs in medical coding. Certifications from organizations like the American Academy of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA) are valuable for career advancement and ensuring proficiency.
- Remote Coding OpportunitiesThe rise of remote work provides new opportunities for medical coders in Nevada. Remote coding positions offer flexibility and can help address the shortage of coders by expanding job opportunities beyond local healthcare facilities. This trend also supports work-life balance and job satisfaction for coders.
- Professional DevelopmentContinuous professional development is essential for coders to stay current with industry changes and advancements. Workshops, webinars, and conferences offer valuable learning opportunities and help coders maintain their credentials and enhance their expertise.
- Technology IntegrationEmbracing advanced coding software and technologies can improve efficiency and accuracy in medical coding. Tools such as artificial intelligence, data analytics, and updated coding systems can streamline coding processes and reduce errors. Healthcare facilities in Nevada can benefit from investing in these technologies to enhance overall coding practices.
Medical coding in Nevada is a dynamic and evolving field that supports the effective operation of the healthcare system across the state. While challenges such as a shortage of qualified coders and the complexity of coding systems exist, there are also significant opportunities for growth and improvement. By investing in education, embracing remote work, and leveraging technology, Nevada can address these challenges and enhance the effectiveness of its medical coding practices. As the healthcare landscape continues to change, medical coders will play a crucial role in ensuring accurate documentation, compliance, and efficient reimbursement processes.
Please read these grant funding steps for Nevada!
What’s the process to apply for Funding in the State of Nevada?
- Find your closest workforce location by visiting the following link: https://nevadaworks.com/
- Under Find Free Job Training & Other Services click on the location closest to your current residence

- Contact your closest local workforce and request eligibility screening for a WIOA Grant for training (WRITE DOWN YOUR ASSIGNED CASE WORKERS NAME & EMAIL AS YOU WILL NEED THAT FOR THE NEXT STEP)
- Click on the link below and complete it to its entirety. This link will create your Proposal & Acceptance letter that you need to provide to your Caseworker. NOTE: Start Date needs to be at least 2 weeks from today’s date https://codingclarified.com/proposal-and-acceptance-pdf-form/
NOTE: CIP CODE 51.0713 (Provide this to your Caseworker upon request)
Click the following link to locate CIP Code for informational purpose: CIP Code Search Here
Title: Medical Insurance Coding Specialist/Coder.
Definition: A program that prepares individuals to perform specialized data entry, classification, and record-keeping procedures related to medical diagnostic, treatment, billing, and insurance documentation. Includes instruction in medical records and insurance software applications, basic anatomy and physiology, medical terminology, fundamentals of medical science and treatment procedures, data classification and coding, data entry skills, and regulations relating to Medicare and insurance documentation.
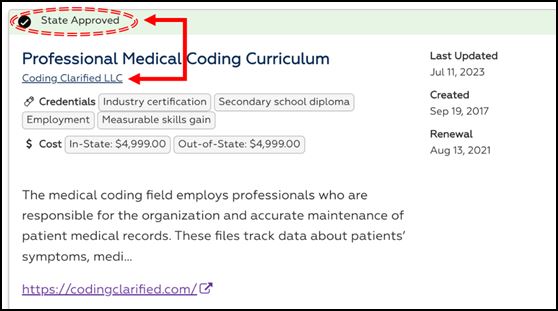
How to verify Coding Clarified is an APPROVED training provider in your state using a reciprocal agreement with AZ
- Click on the following link: https://detr.nv.gov/Page/Training_Providers_List_(Approved)
- Click on Arizona and Nevada to review the Reciprocal agreement or click HERE
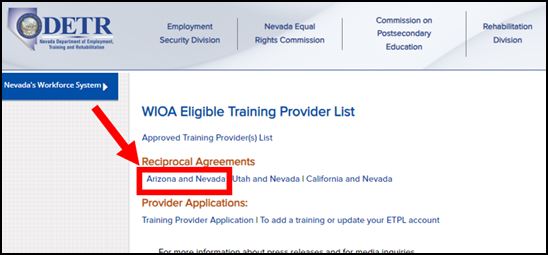
- Next, you can review our approval for the AZ WIOA at the following link: AZ JOB Connection / NV Approved
If you run into any difficulties or your local workforce office has any questions please have them contact Coding Clarified by email [email protected] or 833-633-2633. **Email is preferred**