Billing and Medical Coding for Chronic Kidney Disease (CKD) Guidelines
Chronic Kidney Disease (CKD) is a progressive condition characterized by the gradual loss of kidney function over time. CKD is a critical health concern globally, often caused by diabetes, hypertension, or other factors, and it can lead to severe complications such as end-stage renal disease (ESRD), heart disease, and kidney failure. Proper billing and medical coding for Chronic Kidney Disease is essential to ensure accurate diagnosis, appropriate treatment, and correct reimbursement from insurance providers.
This blog outlines the coding and billing guidelines for Chronic Kidney Disease (CKD), covering ICD-10-CM diagnosis codes, proper sequencing, special considerations, and billing practices.
Understanding Chronic Kidney Disease (CKD)
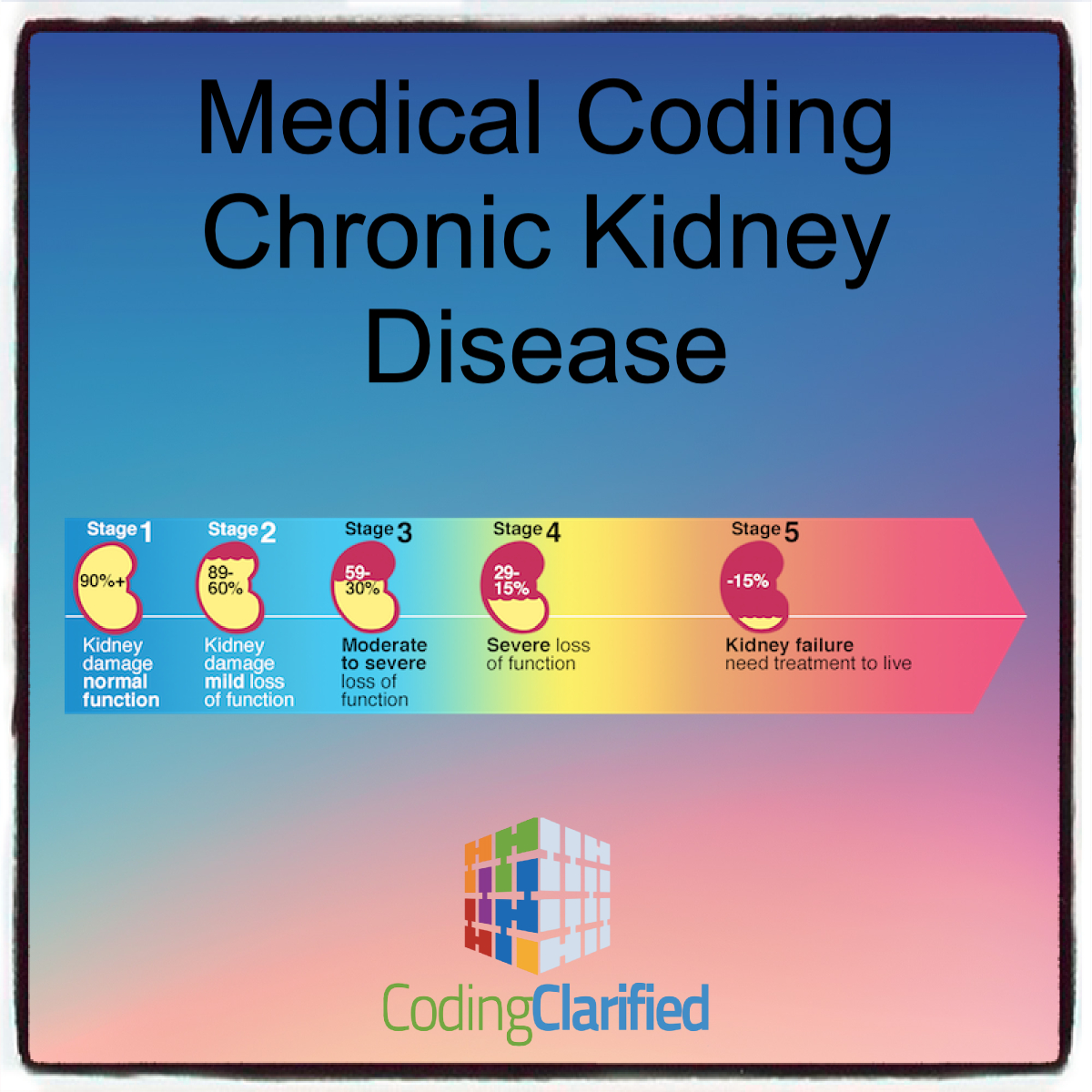
Chronic Kidney Disease refers to a gradual decline in kidney function, typically measured by the glomerular filtration rate (GFR), and is classified into five stages based on the severity of kidney damage.
- Stage 1: Kidney damage with normal or increased GFR (90 mL/min or more)
- Stage 2: Kidney damage with mild reduction in GFR (60-89 mL/min)
- Stage 3: Moderate reduction in GFR (30-59 mL/min)
- Stage 4: Severe reduction in GFR (15-29 mL/min)
- Stage 5: Kidney failure (GFR less than 15 mL/min), often requiring dialysis or kidney transplant
ICD-10-CM Coding for Chronic Kidney Disease
The ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) provides specific codes for CKD based on its stage and underlying causes. https://codingclarified.com/medical-coding-steps-for-icd-10-cm/
Code Range for Chronic Kidney Disease (CKD)
- N18.1: Chronic kidney disease, stage 1
- N18.2: Chronic kidney disease, stage 2
- N18.3: Chronic kidney disease, stage 3
- N18.4: Chronic kidney disease, stage 4
- N18.5: Chronic kidney disease, stage 5
- N18.6: End-stage renal disease (ESRD)
It is important to note that CKD codes are used in conjunction with codes for the underlying conditions (e.g., diabetes mellitus or hypertension) if those conditions are contributing to the CKD.
Stage-Specific Codes
The stage of CKD is a critical component for accurate coding. Documentation should reflect the stage of kidney disease based on the patient’s glomerular filtration rate (GFR), as this helps determine the appropriate code.
For example:
- Stage 1 CKD is defined by a normal or increased GFR (90 mL/min or more), but kidney damage is present. The appropriate code is N18.1.
- Stage 5 CKD (end-stage renal disease) is coded N18.5, and is usually accompanied by additional codes for dialysis (e.g., Z99.2 for dependence on dialysis) or kidney transplant codes (e.g., Z94.0 for kidney transplant status).
CKD and Related Conditions
In many cases, CKD is caused by diabetes (E08-E13) or hypertension (I10-I15), and coders need to capture these underlying conditions as additional diagnoses. In such cases, the coder should always ensure that both the underlying cause and the stage of CKD are captured.
Example:
- E11.22: Type 2 diabetes with diabetic nephropathy (diabetic kidney disease)
- I12.9: Hypertensive heart and chronic kidney disease, stage 1-4, without heart failure
Coding for End-Stage Renal Disease (ESRD)
End-stage renal disease (ESRD) occurs when the kidneys can no longer maintain the body’s balance of fluids, electrolytes, and waste products. It often requires dialysis or a kidney transplant. The ICD-10 code for ESRD is N18.6, and this code should be used when the kidney function has declined to the point of requiring either dialysis or a transplant.
In cases of dialysis, additional codes for dialysis status must be included:
- Z99.2: Dependence on dialysis
If the patient has received a kidney transplant, the following code should be included:
- Z94.0: Kidney transplant status
Sequencing CKD Codes
Proper sequencing of CKD codes is essential for accurate medical billing and insurance reimbursement. Coders should follow these principles:
- Primary Diagnosis: When CKD is the main reason for the patient’s visit or admission, it should be listed as the primary diagnosis. The code for the stage of CKD (e.g., N18.4 for Stage 4 CKD) is the primary diagnosis. If the patient is in end-stage renal disease (ESRD) and requires dialysis or kidney transplant, N18.6 should be the primary diagnosis.
- Underlying Conditions: If the CKD is due to diabetes (E08–E13) or hypertension (I10–I15), the appropriate codes for these conditions must be added as secondary diagnoses. These codes should be sequenced based on the clinical documentation.
Example 1:
-
- Primary Diagnosis: N18.4 (Chronic kidney disease, stage 4)
- Secondary Diagnosis: E11.22 (Type 2 diabetes mellitus with diabetic nephropathy)
Example 2:
-
- Primary Diagnosis: I12.9 (Hypertensive heart and chronic kidney disease, stage 1-4, without heart failure)
- Secondary Diagnosis: N18.3 (Chronic kidney disease, stage 3)
- Dialysis and Kidney Transplantation: If the patient is undergoing dialysis or has received a kidney transplant, the code for ESRD (N18.6) should be listed first, followed by the appropriate dialysis or transplant codes (e.g., Z99.2, Z94.0).Example:
- Primary Diagnosis: N18.6 (End-stage renal disease)
- Secondary Diagnosis: Z99.2 (Dependence on dialysis)
Special Considerations in CKD Coding
Acute Kidney Injury vs. Chronic Kidney Disease
It is critical to distinguish between acute kidney injury (AKI) and chronic kidney disease (CKD), as they are treated differently and require separate coding. AKI is typically coded using N17 codes (e.g., N17.9, acute kidney failure, unspecified). Ensure that documentation clearly distinguishes whether the kidney damage is acute or chronic.
Staging and GFR Values
The glomerular filtration rate (GFR) is a key measure used to determine the stage of CKD. Coders should ensure that the stage of CKD is clearly documented in the clinical record, with the GFR values included. If GFR is not documented, coders may need to query the provider for clarification.
Hypertensive Heart and Kidney Disease
Patients with hypertensive heart and chronic kidney disease should be coded using both the hypertension code (e.g., I12.9) and the appropriate CKD stage code (e.g., N18.4). Ensure that both conditions are clearly documented and sequenced in the correct order.
Billing Considerations for CKD
- Evaluation and Management (E/M) Services: When billing for E/M services, such as office visits, the complexity of the visit may be based on the stage of CKD and any comorbidities, such as diabetes or heart disease. The CPT code for the office visit (e.g., 99213 for an established patient) should reflect the complexity of the patient’s condition.
- Dialysis and Transplant Services: If the patient requires dialysis, additional CPT codes for dialysis procedures (e.g., 90935 for hemodialysis) should be used. For kidney transplant patients, the appropriate post-transplant care codes should be billed, such as 99371-99373 for post-transplant management.
- Chronic Disease Management: For patients with CKD, chronic care management (CCM) services may be billed under the CPT codes 99439-99441 for remote monitoring, care coordination, and long-term management of the disease.
Correct coding and billing for Chronic Kidney Disease (CKD) are essential for accurate diagnosis, treatment, and reimbursement. By following the ICD-10-CM guidelines for CKD staging, properly sequencing codes, and documenting underlying conditions, coders can help healthcare providers avoid errors and ensure proper reimbursement for CKD-related care. It is also critical to consider comorbid conditions such as diabetes and hypertension, which often play a significant role in CKD. By adhering to these guidelines, medical professionals can improve care coordination and patient outcomes while ensuring compliance with coding and billing requirements.