Guidelines for Medical Coding and Casual Relationships Between Diabetes, Hypertension, and Chronic Kidney Disease in Medical Coding
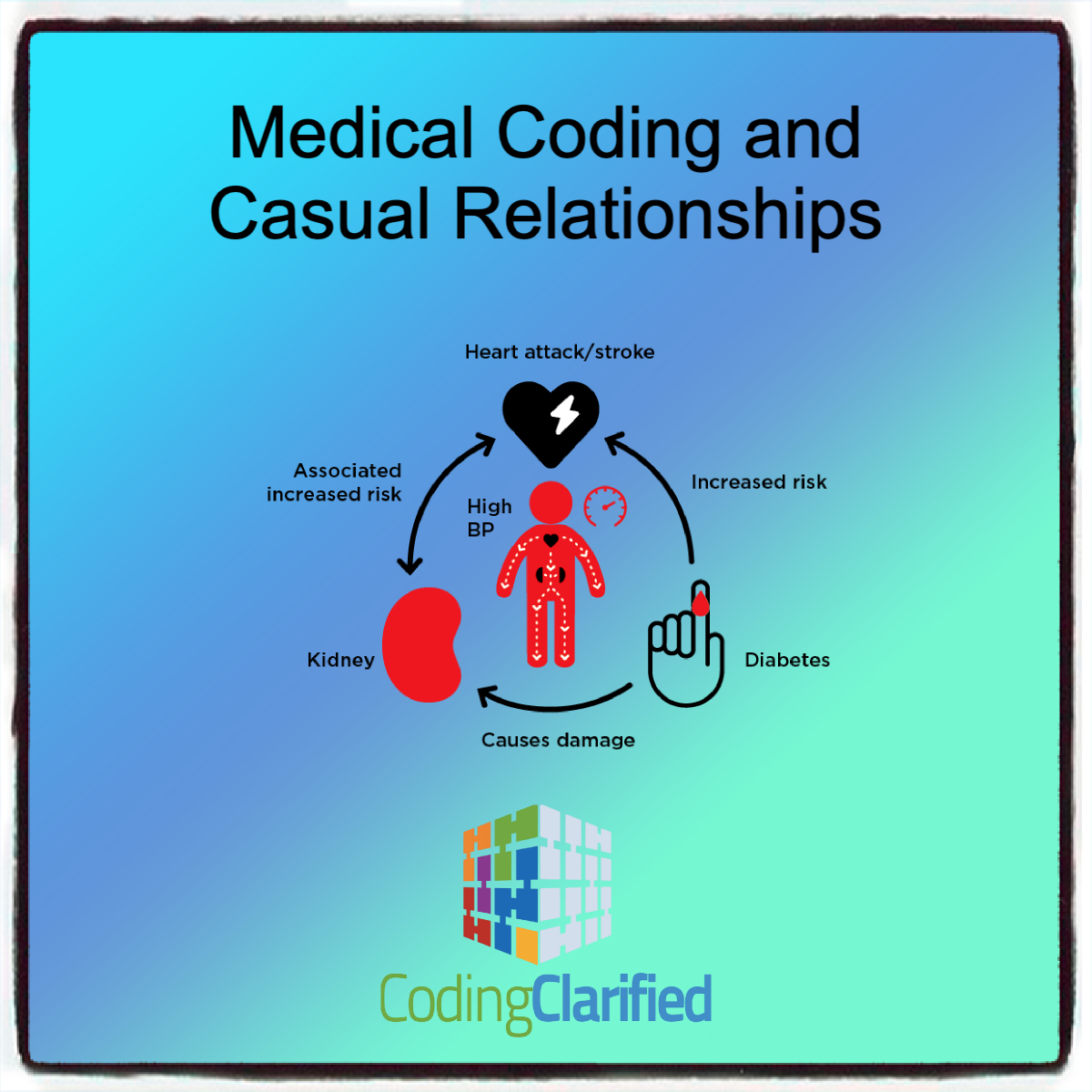
Medical coding plays a crucial role in ensuring accurate billing, proper diagnosis, and clear communication between healthcare providers and insurers. For patients with multiple chronic conditions, medical coding and casual relationships such as diabetes mellitus, hypertension, and chronic kidney disease (CKD) can be complex. These conditions often interact and affect one another, requiring coders to be familiar with how to appropriately represent their relationship in coding systems like ICD-10-CM.
In this blog, we’ll explore the guidelines for coding casual relationships between diabetes, hypertension, and chronic kidney disease, focusing on how to correctly assign codes to reflect these interconnected conditions.
When “With” Assumes a Causal Relationship
ICD-10-CM guidelines, Section I. A.15, says, “The classification presumes a causal relationship between the two conditions linked by these terms [i.e., “with”] in the Alphabetic Index or Tabular List.” In other words, you may presume a relationship between two conditions if those conditions are linked within the ICD-10-CM Alphabetic Index or Tabular List — even if the documentation does not explicitly state that the two conditions are related.
Understanding the Relationship Between Diabetes, Hypertension, and Chronic Kidney Disease
When coding for the relationship between diabetes mellitus, hypertension, and chronic kidney disease, it is important to recognize that these conditions are frequently interrelated.
- Diabetes and Hypertension: Both conditions often coexist, and the combination of uncontrolled diabetes and high blood pressure can significantly increase the risk of developing chronic kidney disease. Hypertension is a common cause of kidney damage in patients with diabetes, and both conditions can worsen kidney function over time.
- Diabetes and Chronic Kidney Disease: Diabetes, particularly type 2 diabetes, is one of the leading causes of chronic kidney disease. High blood sugar levels can damage blood vessels in the kidneys, leading to kidney dysfunction. This is often referred to as diabetic nephropathy.
- Hypertension and Chronic Kidney Disease: High blood pressure can cause or exacerbate kidney damage, and kidney disease can, in turn, worsen hypertension due to the kidneys’ role in regulating blood pressure.
The casual relationship between these conditions means that while they are often interlinked, not every case of chronic kidney disease is directly caused by diabetes or hypertension, and vice versa. However, coders must be careful to reflect the clinical relationship based on the provider’s documentation.
Key Coding Guidelines for Diabetes, Hypertension, and Chronic Kidney Disease
The ICD-10-CM coding system provides specific codes to represent these conditions, and the relationship between them must be documented clearly in the medical record. Below are guidelines for selecting the correct codes:
Diabetes Codes (E08–E13)
There are several types of diabetes, and it’s important to code correctly based on the type and whether there is any associated kidney disease.
- Type 1 Diabetes (E10): When coding for Type 1 diabetes, the condition may lead to diabetic nephropathy, so the coder needs to ensure that the kidney disease is identified with the correct code.
- Type 2 Diabetes (E11): Type 2 diabetes is more commonly associated with chronic kidney disease. When coding for Type 2 diabetes, coders should identify the presence of diabetic nephropathy (E11.21 for Type 2 diabetes with diabetic nephropathy).Example Codes for Diabetes:
- E11.9: Type 2 diabetes mellitus without complications
- E11.21: Type 2 diabetes mellitus with diabetic nephropathy (i.e., kidney disease related to diabetes) https://codingclarified.com/medical-coding-diabetes/?fbclid=IwZXh0bgNhZW0CMTEAAR1wn6_N161IwuLW9wKqWVtdYTs6aPLNtCCo9bbPLcRqGIOxR-WSZFidI-0_aem_JwOfl1KLzzbK0t-jzQl_KQ
Here’s a list of the associated diabetic conditions where the link is assumed in ICD-10-CM:
- amyotrophy
- arthropathy NEC
- autonomic (poly) neuropathy
- cataract
- Charcot’s joints
- chronic kidney disease
- circulatory complication NEC
- complication
- specified NEC
- dermatitis
- foot ulcer
- gangrene
- gastroparalysis
- gastroparesis
- glomerulonephrosis, intracapillary
- glomerulosclerosis, intercapillary
- hyperglycemia
- hyperosmolarity
- with coma
- hypoglycemia
- with coma
- ketoacidosis
- with coma
- kidney complications NEC
- Kimmelsteil-Wilson disease
- loss of protective sensation(LOPS) – see Diabetes, by type, with neuropathy
- mononeuropathy
- myasthenia
- necrobiosis lipoidica
- nephropathy
- neuralgia
- neurologic complication NEC
- neuropathic arthropathy
- neuropathy
- ophthalmic complication NEC
- oral complication NEC
- osteomyelitis
- periodontal disease
- peripheral angiopathy
- with gangrene
- polyneuropathy
- renal complication NEC
- renal tubular degeneration
- retinopathy
- skin complication NEC
- skin ulcer NEC
Hypertension Codes (I10–I15)
Hypertension (high blood pressure) can contribute to both kidney damage and worsened kidney function. When coding for hypertension, it’s important to specify whether the hypertension is primary or secondary (due to another condition, such as chronic kidney disease).
- Essential Hypertension (I10): This is the most common form of hypertension and is often a contributing factor to kidney disease in patients with diabetes.
- Hypertensive Heart and Chronic Kidney Disease (I13): If a patient has hypertension that is causing kidney damage or heart failure, the appropriate code should reflect the combination of these conditions.Example Codes for Hypertension:
- I10: Essential (primary) hypertension
- I13.10: Hypertensive heart AND chronic kidney disease, stage 1-4, without heart failure
- I13.11: Hypertensive heart AND chronic kidney disease, stage 1-4, with heart failure
Chronic Kidney Disease Codes (N18)
The stage of chronic kidney disease must be specified to determine the appropriate code. Chronic kidney disease (CKD) is categorized into stages based on the level of kidney function.
- CKD Stage 1-5: The stages are defined by the glomerular filtration rate (GFR). For example, stage 1 refers to kidney disease with normal or elevated GFR (≥ 90), and stage 5 refers to kidney failure with a GFR < 15.
- Diabetic Nephropathy and Hypertensive Nephropathy: If CKD is due to diabetes or hypertension, coders should include the diabetes or hypertension code along with the appropriate CKD stage.Example Codes for Chronic Kidney Disease:
- N18.1: Chronic kidney disease, stage 1 (usually combined with diabetes or hypertension code if appropriate)
- N18.5: Chronic kidney disease, stage 5 (end-stage kidney failure, often requiring dialysis)
Sequencing of Codes
The sequence in which codes are assigned can impact the clinical meaning and the payment outcome. When coding multiple conditions like diabetes, hypertension, and chronic kidney disease, sequencing follows certain guidelines:
- Primary Diagnosis: Typically, the primary condition responsible for the patient’s visit or admission should be listed first. If the patient is being treated for diabetic nephropathy, for example, the diabetes code (e.g., E11.21) would generally be listed first, followed by the CKD code (e.g., N18.1 or N18.5) to reflect the severity of the kidney disease.
- Hypertension as a Secondary Diagnosis: If hypertension is a contributing factor to CKD or diabetes, it may be listed as a secondary diagnosis (e.g., I10 or I13). In cases where hypertension is causing kidney disease, the hypertension code should appear before the CKD code.Example Sequencing:
- Primary diagnosis: E11.21 (Type 2 diabetes mellitus with diabetic nephropathy)
- Secondary diagnosis: N18.4 (Chronic kidney disease, stage 4)
- Additional diagnosis: I10 (Essential hypertension)
Special Considerations and Common Coding Errors
Comorbidity or “Casual” Relationships
It’s important to note that while diabetes, hypertension, and chronic kidney disease are often seen together, they are not always causally related. For example, a patient may have hypertension but no kidney damage or a different cause of kidney disease unrelated to their diabetes. Coders should always verify with clinical documentation whether these conditions are causally related or whether they are simply comorbidities that exist alongside one another.
Chronic Kidney Disease and Dialysis
When a patient with CKD progresses to end-stage renal disease (ESRD) and requires dialysis, this must be clearly documented, as dialysis codes (e.g., V45.1 or Z99.2) will also apply. Make sure to avoid confusion between patients who are in the earlier stages of CKD and those on dialysis.
Accurately coding the casual relationships between diabetes, hypertension, and chronic kidney disease is essential for proper diagnosis, treatment, and reimbursement. Coders must carefully review the clinical documentation to understand how these conditions interrelate and apply the appropriate ICD-10-CM codes accordingly.
By following these guidelines, ensuring correct code sequencing, and verifying the documentation with providers, coders can help healthcare organizations avoid coding errors, reduce claim denials, and ensure that patients receive the appropriate care for their complex medical conditions.