Understanding Pain ICD-10 Coding: Key Codes and Guidelines
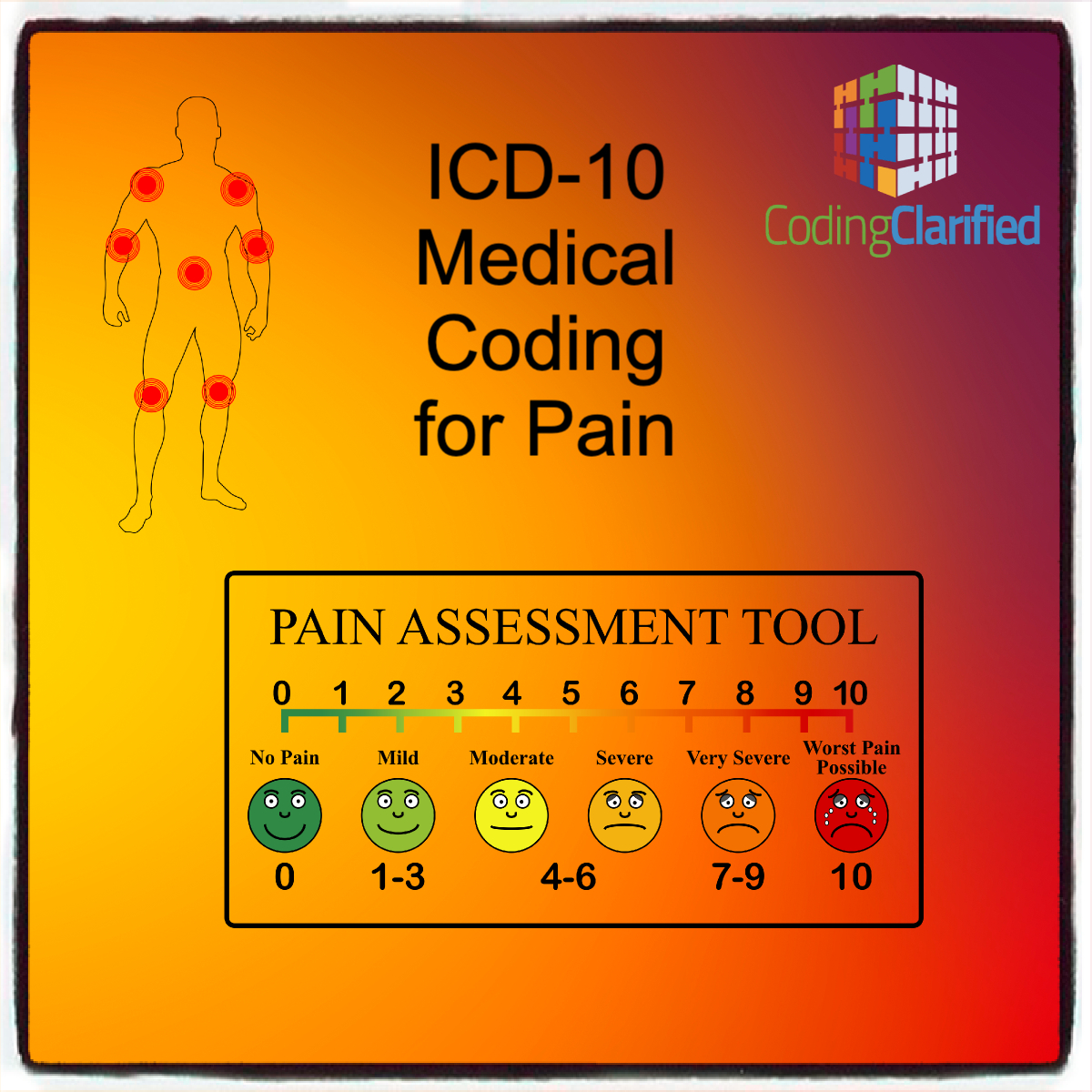
Medical coding for pain is a critical aspect of healthcare documentation and billing. Accurate coding ensures that healthcare providers are properly reimbursed for their services and that patient records reflect their true condition. The ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) provides a comprehensive system for classifying and coding diagnoses, including various types of pain. This article explores the nuances of coding pain in ICD-10-CM, including key codes, coding guidelines, and best practices.
What is ICD-10-CM
ICD-10-CM is a medical coding system used in the United States for classifying and coding diagnoses. It includes detailed codes for a wide range of conditions, including pain, which is categorized based on its type, location, and duration.
Pain coding in ICD-10-CM requires specificity to ensure accurate documentation and billing. The ICD-10-CM diagnosis code for unspecified pain is R52 This code can be used for acute pain, generalized pain, or pain that is not otherwise specified. However, it does not apply to pain disorders that are exclusively related to psychological factors, or acute and chronic pain that is not classified elsewhere.
When a patient’s visit or service is specifically for pain management or pain control, the G89 category codes should be listed first. This is because the provider is treating the pain, not the underlying condition. When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source. The ICD-10-CM guidelines state that if the cause of the pain is known, you should assign a code for the underlying diagnosis, not the pain code.
Only report pain diagnosis codes from the G89 category as the primary diagnosis when:
- The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or
- The reason for the service is for pain control or pain management.
If the purpose of the encounter is to manage the pain rather than the underlying condition, then you should assign a pain code and sequence it first.
What are the Different Types of ICD-10 Pain Codes
You can find pain codes in three different places in the ICD-10-CM manual:
- Pain that points to a disorder of a specific body system is classified in the body system chapters. For example, low back pain is classified in the Musculoskeletal chapter (M54.5) and testicular pain is classified in the Genitourinary System chapter (N50.8).
- Pain that does not point to a specific body system is classified in the Symptoms and Signs chapter. For example, abdominal pain is classified to category R10.
- Certain specific types of pain are classified to category G89 (Pain, not elsewhere classified) in the Nervous System chapter
Central pain syndrome is defined by the National Institute of Neurological Disorders and Stroke (NINDS) as “a neurological condition caused by damage to or dysfunction of the central nervous system.” Central pain syndrome can occur as a result of stroke, multiple sclerosis, neoplasm, epilepsy, CNS trauma, or Parkinson’s disease. Patients with central pain syndrome may experience localized pain, burning, and/or numbness in specific parts of the body, or throughout the body. ICD-10-CM classifies central pain syndrome to code G89.0 (Central pain syndrome).
Chronic pain syndrome is chronic pain associated with significant psychosocial dysfunction. The psychosocial problems may include depression, drug dependence, complaints that are out of proportion to the physical findings, anxiety, and other manifestations. Chronic pain syndrome is not synonymous with chronic pain. You should code this condition only when the physician specifically documents it. Chronic pain syndrome is reported with code G89.4 (Chronic pain syndrome).
Pain Medical Coding ICD-10: Specific Conditions and Codes
- Pain, General
- R52.9: Pain, unspecified
- This code is used when the type or location of pain is not specified. It is a broad category and should be used when no more specific code is available.
- Acute Pain
- G89.11: Acute pain due to trauma
- G89.12: Acute pain due to other external causes
- G89.18: Other acute pain
- Acute pain codes are used for pain that has a sudden onset and is typically associated with injury or surgery.
- Chronic Pain
- G89.21: Chronic pain due to trauma
- G89.22: Chronic pain due to other external causes
- G89.29: Other chronic pain
- Chronic pain codes are used for pain that persists over a longer period, often beyond the expected recovery time from an injury or illness.
- Pain Due to Cancer
- G89.3: Neoplasm-related pain
- This code is used for pain associated with malignancies, either due to the cancer itself or as a side effect of cancer treatment.
- Pain Related to Specific Conditions
- M79.1: Myalgia (muscle pain)
- M54.5: Low back pain
- M25.5: Pain in joint (for specific joints)
- These codes are used when pain is linked to a specific condition or anatomical site, such as muscle pain or joint pain.
ICD-10 Guidelines for Chronic Pain Management
- Be Specific: Accurate pain coding requires specific details about the type, location, and duration of pain. Vague codes like R52.9 (Pain, unspecified) should be avoided when more specific codes are available.
- Document Thoroughly: Detailed documentation by the healthcare provider is essential for accurate coding. The medical record should include information on the pain’s onset, location, severity, and any associated conditions.
- Consider the Underlying Cause: If pain is a symptom of another condition, such as a chronic disease or injury, use codes that reflect both the pain and the underlying cause. For instance, use G89.22 (Chronic pain due to other external causes) along with the code for the underlying condition.
- Use Combination Codes When Applicable: Some codes, like those for pain due to cancer, combine the diagnosis of the underlying condition with the symptom of pain, which helps streamline coding and ensures accurate representation of the patient’s condition.
- Follow Official Guidelines: Always refer to the latest ICD-10-CM coding guidelines and updates to ensure compliance and accuracy. Coding conventions and guidelines may change, so staying informed is crucial.
ICD10-CM Guidelines
Pain – Category G89
1) General coding information Codes in category G89, Pain, not elsewhere classified, may be used in conjunction with codes from other categories and chapters to provide more detail about acute or chronic pain and neoplasm-related pain, unless otherwise indicated below. If the pain is not specified as acute or chronic, post-thoracotomy, postprocedural, or neoplasm-related, do not assign codes from category G89.
A code from category G89 should not be assigned if the underlying (definitive) diagnosis is known, unless the reason for the encounter is pain control/ management and not management of the underlying condition.
When an admission or encounter is for a procedure aimed at treating the underlying condition (e.g., spinal fusion, kyphoplasty), a code for the underlying condition (e.g., vertebral fracture, spinal stenosis) should be assigned as the principal diagnosis. No code from category G89 should be assigned. (a) Category G89 Codes as Principal or First-Listed Diagnosis Category G89 codes are acceptable as principal diagnosis or the first-listed code:
- When pain control or pain management is the reason for the admission/encounter (e.g., a patient with displaced intervertebral disc, nerve impingement and severe back pain presents for injection of steroid into the spinal canal). The underlying cause of the pain should be reported as an additional diagnosis, if known.
- When a patient is admitted for the insertion of a neurostimulator for pain control, assign the appropriate pain code as the principal or first-listed diagnosis. When an admission or encounter is for a procedure aimed at treating the underlying condition and a neurostimulator is inserted for pain control during the same admission/encounter, a code for the underlying condition should be assigned as the principal diagnosis and the appropriate pain code should be assigned as a secondary diagnosis.
(b) Use of Category G89 Codes in Conjunction with Site Specific Pain Codes
(i) Assigning Category G89 and Site-Specific Pain Codes Codes from category G89 may be used in conjunction with codes that identify the site of pain (including codes from chapter 18) if the category G89 code provides additional information. For example, if the code describes the site of the pain, but does not fully describe whether the pain is acute or chronic, then both codes should be assigned.
(ii) Sequencing of Category G89 Codes with Site-Specific
Pain Codes
The sequencing of category G89 codes with site- specific pain codes (including chapter 18 codes), is dependent on the circumstances of the encounter/admission as follows:
- If the encounter is for pain control or pain management, assign the code from category G89 followed by the code identifying the specific site of pain (e.g., encounter for pain management for acute neck pain from trauma is assigned code G89.11, Acute pain due to trauma, followed by code M54.2, Cervicalgia, to identify the site of pain).
- If the encounter is for any other reason except pain control or pain management, and a related definitive diagnosis has not been established (confirmed) by the provider, assign the code for the specific site of pain first, followed by the appropriate code from category G89. 2) Pain due to devices, implants and grafts See Section I.C.19. Pain due to medical devices 3) Postoperative Pain The provider’s documentation should be used to guide the coding of postoperative pain, as well as Section III. Reporting Additional Diagnoses and Section IV. Diagnostic Coding and Reporting in the Outpatient Setting. The default for post-thoracotomy and other postoperative pain not specified as acute or chronic is the code for the acute form. Routine or expected postoperative pain immediately after surgery should not be coded. (a) Postoperative pain not associated with specific postoperative complication Postoperative pain not associated with a specific postoperative complication is assigned to the appropriate postoperative pain code in category G89. (b) Postoperative pain associated with specific postoperative complication Postoperative pain associated with a specific postoperative complication (such as painful wire sutures) is assigned to the appropriate code(s) found in Chapter 19, Injury, poisoning, and certain other consequences of external causes. If appropriate, use additional code(s) from category G89 to identify acute or chronic pain (G89.18 or G89.28). 4) Chronic pain Chronic pain is classified to subcategory G89.2. There is no time frame defining when pain becomes chronic pain. The provider’s documentation should be used to guide use of these codes. 5) Neoplasm Related Pain Code G89.3 is assigned to pain documented as being related, associated or due to cancer, primary or secondary malignancy, or tumor. This code is assigned regardless of whether the pain is acute or chronic. This code may be assigned as the principal or first-listed code when the stated reason for the admission/encounter is documented as pain control/pain management. The underlying neoplasm should be reported as an additional diagnosis. When the reason for the admission/encounter is management of the neoplasm and the pain associated with the neoplasm is also documented, code G89.3 may be assigned as an additional diagnosis. It is not necessary to assign an additional code for the site of the pain. See Section I.C.2. for instructions on the sequencing of neoplasms for all other stated reasons for the admission/encounter (except for pain control/pain management). 6) Chronic pain syndrome Central pain syndrome (G89.0) and chronic pain syndrome (G89.4) are different than the term “chronic pain,” and therefore codes should only be used when the provider has specifically documented this condition. See Section I.C.5. Pain disorders related to psychological factors
https://www.cms.gov/files/document/fy-2025-icd-10-cm-coding-guidelines.pdf
Best Practices for Pain Medical Coding
- Regular Training: Healthcare providers and coders should undergo regular training to stay updated on ICD-10-CM changes and best practices for pain coding.
- Audit and Review: Regular audits of coding practices can help identify and correct errors, ensuring that pain-related diagnoses are coded accurately and consistently.
- Collaborate with Providers: Effective communication between coders and healthcare providers is essential. Coders should clarify any ambiguities in the documentation to ensure accurate coding.
- Use Coding Resources: Leverage coding manuals, software tools, and online resources to assist with accurate pain coding. Many resources offer detailed guidance and examples for complex coding scenarios.
Pain coding in ICD-10-CM is a critical component of medical coding that requires precision and attention to detail. By understanding the specific codes for various types of pain, adhering to coding guidelines, and implementing best practices, healthcare professionals can ensure accurate documentation and billing. This not only supports proper reimbursement but also enhances patient care by providing a clear and detailed record of their pain and related conditions.