Understanding the Medicare 8-Minute Rule for Medical Coding
Medical coding is a critical aspect of healthcare administration, ensuring that services rendered are accurately translated into codes for billing and reimbursement purposes. For Medicare patients, the 8-minute rule plays a significant role in determining how time-based services are coded and billed. This guideline affects how healthcare providers document and submit claims for services that are based on time, particularly in physical therapy, occupational therapy, and speech-language pathology.
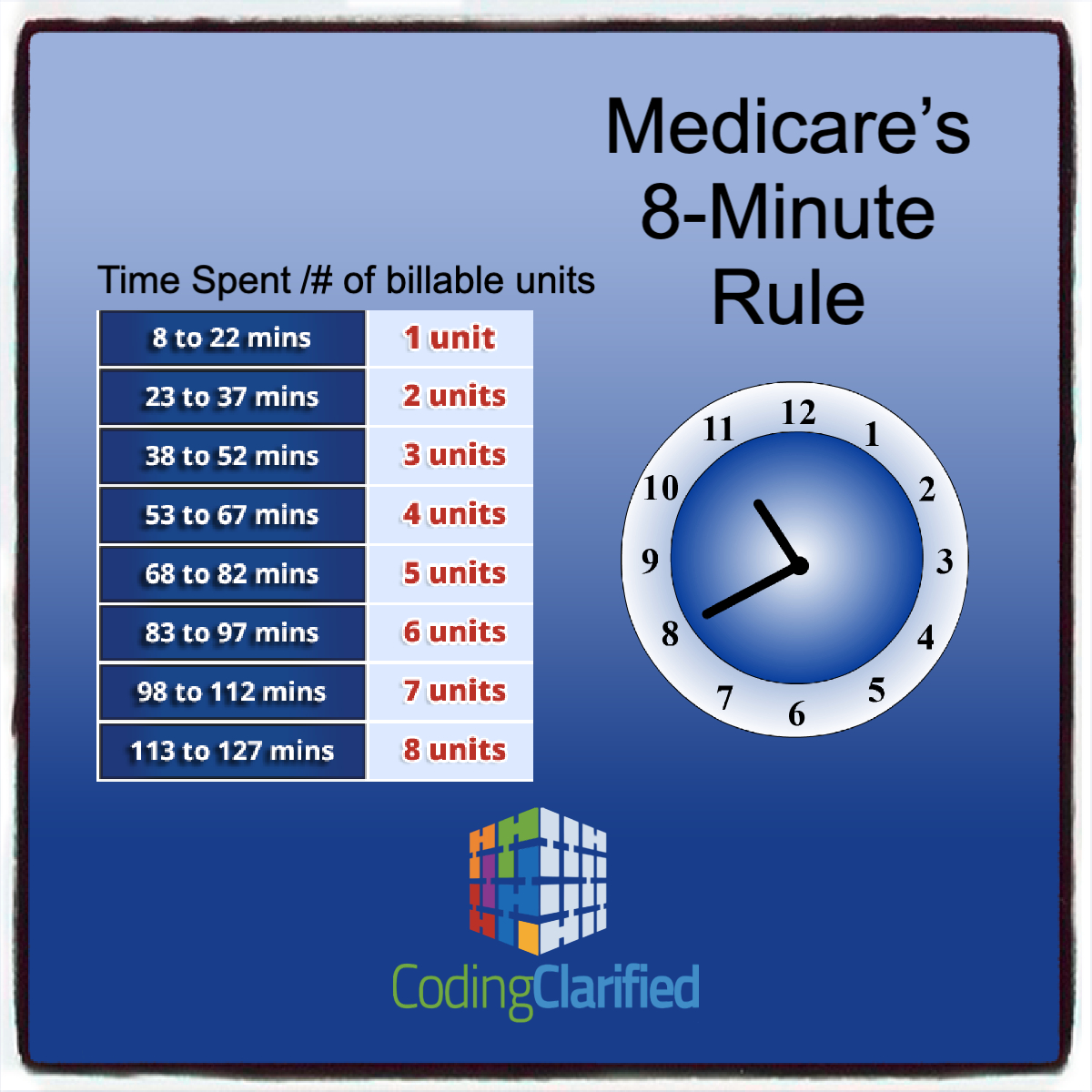
The rule allows practitioners to bill Medicare for one unit of service if its length is at least eight (but fewer than 22) minutes. A billable “unit” of service refers to the time interval for the service. Under the 8-minute rule, units of service consist of 15 minutes each.
What is the 8-Minute Rule?
The 8-minute rule is a guideline used by Medicare to determine how to appropriately bill for time-based therapy services. According to Medicare guidelines, services are billed based on the amount of time spent providing direct patient care. The 8-minute rule helps translate the total time spent into billable units, ensuring accurate and fair compensation for the services provided.
For time-based codes, you must provide direct treatment for at least eight minutes in order to receive reimbursement from Medicare. Basically, when calculating the number of billable units for a particular date of service, Medicare adds up the total minutes of skilled, one-on-one therapy and divides that total by 15. If eight or more minutes are left over, you can bill for one more unit; if seven or fewer minutes remain, you cannot bill an additional unit.
Many times, when you divide the total timed minutes by 15, you get a remainder that includes minutes from more than one service. For example, you might have 5 leftover minutes of therapeutic exercise and 3 leftover minutes of manual therapy. Individually, neither of these remainders meets the 8-minute threshold. When combined, though, they amount to 8 minutes—and per Medicare billing guidelines, that means you can bill one unit of the service with the greatest time total.
The Rule of Eights— is sometimes referred to as the AMA 8-Minute Rule—is a slight variant of CMS’s 8-Minute Rule. The Rule of Eights still counts billable units in 15-minute increments, but instead of combining the time from multiple units, the rule is applied separately to each unique timed service. Therefore, the math is also applied separately. (Keep in mind that the Rule of Eights only applies to timed codes that have 15 minutes listed as the “usual time” in the operational definition of the code.
CPT codes actually do make allowances for assessment and management time. That time includes “all the things you have to do to deliver an intervention,” such as:
- assessing the patient prior to performing a hands-on intervention;
- assessing the patient’s response to the intervention;
- instructing, counseling, and advice-giving about at-home self-care;
- answering patient and/or caregiver questions; and
- documenting in the presence of the patient.
The key to justifying your decision to bill for assessment and management time lies in your documentation. If the documentation is defensible (i.e., it’s thorough, it accurately describes the treatment, it defends the prescriber’s clinical reasoning, and it’s easily understood by another provider), then payers will likely greenlight the extra minutes.
- Time-based (constant attendance) CPT codes: These codes allow for variable billing in 15-minute increments when a practitioner provides a patient with one-on-one services such as therapeutic exercise or manual therapy.
- Service-based (supervised or untimed) CPT codes: These are the codes therapists use to perform services such as conducting an evaluation or applying hot/cold packs. It doesn’t matter if you complete these types of treatments in 5 minutes or 45, because you can only bill one code.
Here are some key points about the 8-minute rule:
-
When it applies
The rule applies to time-based current procedural terminology (CPT) codes for outpatient services.
-
How it works
For services that last between 8 and 22 minutes, providers can bill for a single billable unit. After 22 minutes, billable units are calculated in 15-minute increments.
-
When it doesn’t apply
Services that last less than 8 minutes are not billable.
-
How it’s used
The rule helps ensure accurate reimbursement for outpatient services like physical, occupational, and speech therapy.
-
How it’s documentedPhysical therapists must document the start and end times of each billable activity.While understanding the core principles of the 8-minute rule is essential, many healthcare providers benefit from practical tools and resources that simplify its application in daily practice.Documentation templates, quick-reference charts, and real-world case studies can significantly reduce billing errors and improve compliance.For providers seeking comprehensive resources including calculators and step-by-step documentation examples, a guide to 8-Minute Rule offers actionable tools designed specifically for busy clinical practices.
How the 8-Minute Rule Works
- Calculating Time: The 8-minute rule applies to services provided in 15-minute increments. For instance, if a therapist spends 23 minutes with a patient, this time would be rounded according to the 8-minute rule to determine how many billable units can be claimed.
- Unit Calculation: Under the 8-minute rule, the time spent on therapy is divided by 15 to determine the number of units. However, the rule specifies that only time spent directly interacting with the patient counts toward this calculation. The general breakdown is as follows:
- 8 to 22 minutes: 1 unit
- 23 to 37 minutes: 2 units
- 38 to 52 minutes: 3 units
- 53 to 67 minutes: 4 units
- And so on.
- Documentation: Accurate documentation is essential. Therapists must record the total time spent on therapy and provide detailed notes to justify the billed units. This ensures compliance with Medicare regulations and helps avoid claim denials or audits.
Practical Application and Examples
Let’s explore a few practical examples to illustrate how the 8-minute rule is applied:
- Example 1: A physical therapist spends 18 minutes with a patient. According to the 8-minute rule, the therapist can bill for 1 unit, as the time falls between 8 and 22 minutes.
- Example 2: If the therapist spends 36 minutes, this would be rounded to 2 units, as it falls between 23 and 37 minutes.
- Example 3: A session lasts 50 minutes. Under the 8-minute rule, this time would be billed as 3 units because it falls within the 38 to 52 minutes range.
Implications for Providers
- Accuracy and Compliance: Adhering to the 8-minute rule is crucial for ensuring accurate billing and compliance with Medicare’s requirements. Providers should regularly review their documentation practices to align with these guidelines and avoid potential issues with claim denials or audits.
- Training and Education: Providers should ensure that their staff is well-trained in the 8-minute rule and its application. Ongoing education can help maintain accuracy in billing and improve overall efficiency.
- Impact on Reimbursement: Proper application of the 8-minute rule affects reimbursement rates. Incorrectly calculating or documenting therapy time can lead to underbilling or overbilling, both of which can have financial repercussions for the provider.
The 8-minute rule is an essential guideline for medical coding in the context of Medicare billing for time-based therapy services. By accurately applying this rule, providers can ensure proper reimbursement for their services while maintaining compliance with Medicare regulations. Thorough documentation and adherence to these guidelines not only facilitate smooth billing processes but also support the integrity of healthcare administration. As regulations and guidelines continue to evolve, staying informed and educated about these rules is vital for successful and compliant medical coding practices.