AI is significantly transforming the medical coding and billing industry, improving productivity and efficiency, but human coders remain indispensable for various reasons. Here’s how medical coding productivity and efficiency with AI is enhancing the role of medical coders and why coders will still be essential in the future:
How AI Increases Productivity in Medical Coding and Billing
- Automating Routine Tasks: AI can quickly process vast amounts of patient data, identifying and assigning the correct codes for diagnoses, treatments, and procedures. This reduces the time medical coders spend on repetitive tasks, such as reviewing patient records or looking up codes, allowing them to focus on more complex cases.
- Improved Accuracy: AI algorithms are capable of recognizing patterns and reducing human error, ensuring that codes are assigned more accurately. This helps prevent claim rejections and denials, streamlining the billing process and improving revenue cycle management.
- Faster Turnaround: With AI, coders can process records faster since AI can assist in reviewing, validating, and coding large volumes of medical data at a much higher speed than humans. This leads to quicker claim submissions and faster reimbursement for healthcare providers.
- Enhanced Data Analytics: AI can analyze trends in coding patterns, highlighting any discrepancies, missed codes, or potential fraud. By offering insights, it enables coders to adjust their practices, improve quality, and identify any areas of risk.
- Reduction in Administrative Burden: Many coding and billing jobs involve navigating complex healthcare regulations. AI can assist coders by keeping track of regulatory changes and ensuring compliance, reducing the burden of constantly staying updated on evolving rules.
Why Medical Coders Will Still Be Needed After AI Implementation
- Complex Decision-Making: AI can handle a high volume of routine tasks, but it still lacks the critical thinking and decision-making capabilities that human coders bring. Coders are needed to handle complex cases, such as rare diseases, multi-system diagnoses, or intricate medical procedures that AI might misinterpret or be unable to handle.
- Human Judgment for Context: Medical coding involves not just assigning the correct code, but also understanding the nuances of patient history, treatments, and the clinical context. Coders often apply human judgment in cases where AI might miss subtle, but important, details. For example, understanding why a certain code should be applied based on the patient’s circumstances requires a deep understanding of medical knowledge and patient care that AI cannot fully replicate.
- Adaptation to New or Unusual Situations: While AI can learn and adapt to common patterns, it is often less effective in new or unusual situations. Human coders are better equipped to evaluate new codes, ambiguous clinical documentation, or cases that don’t fit neatly into a set of rules.
- Accountability and Ethical Oversight: Coders often work with confidential patient information, and ensuring compliance with healthcare regulations (like HIPAA in the U.S.) requires ethical oversight. Human coders are responsible for making sure that data is handled properly and that coding practices are consistent with legal requirements. AI systems might still struggle with this oversight role.
- Quality Assurance: AI can assist in coding, but human coders still play an essential role in quality control. Coders can review AI-generated codes for accuracy and verify that they are consistent with clinical documentation. They can also address any discrepancies, ensuring the integrity of the data used for billing and reimbursement.
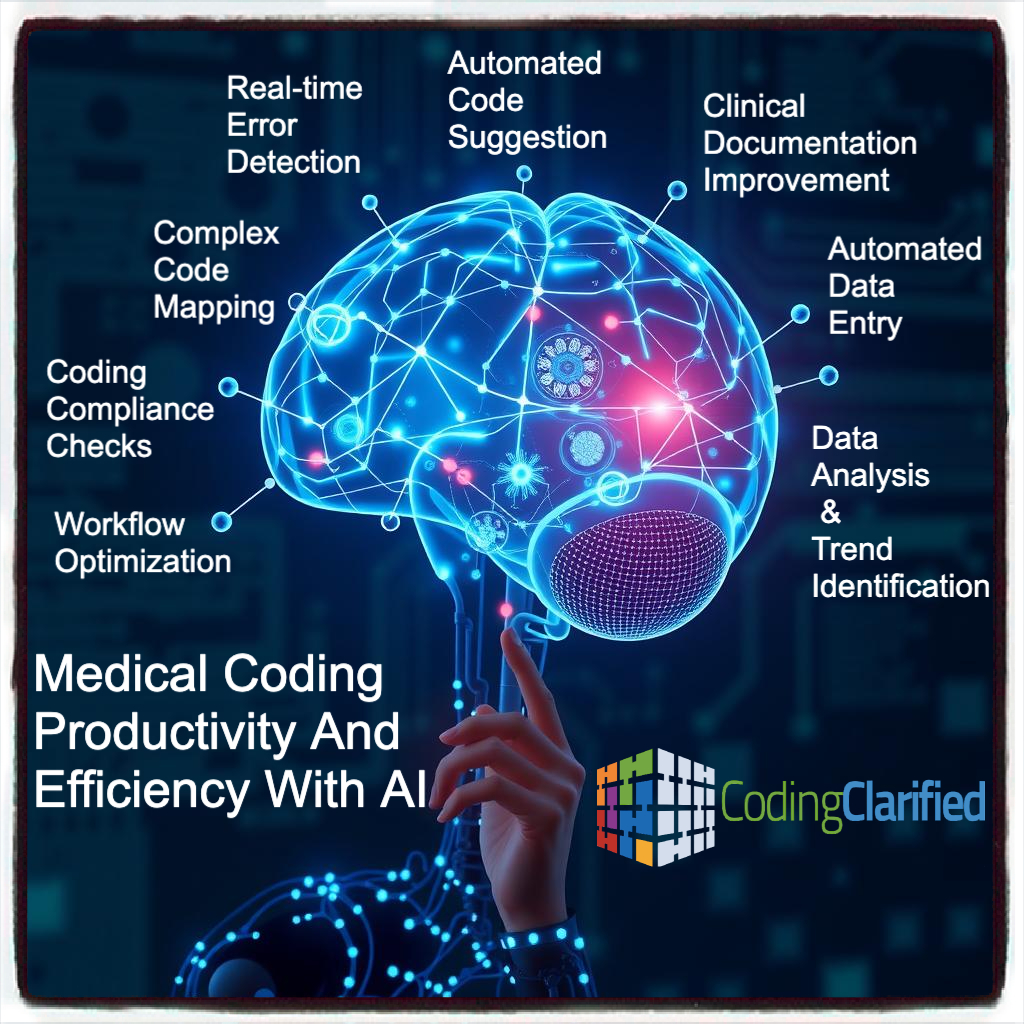
AI can significantly enhance a medical coder’s efficiency by:
-
Automated Code Suggestion:AI algorithms can analyze medical records and suggest the most accurate codes based on the documented clinical information, reducing the time spent searching through coding manuals.
-
Real-time Error Detection:AI can identify potential coding errors as the coder inputs codes, providing immediate feedback and preventing inaccurate claims submission.
-
Clinical Documentation Improvement:AI can analyze medical records and flag areas where documentation is unclear or missing critical details, prompting providers to improve their documentation for accurate coding.
-
Complex Code Mapping:AI can handle intricate coding scenarios, including complex diagnoses and procedures, by cross-referencing different coding systems and providing optimal code selections.
-
Data Analysis and Trend Identification:AI can analyze large datasets of coded medical records to identify patterns and trends, helping healthcare providers make informed decisions about patient care and resource allocation.
-
Coding Compliance Checks:AI can automatically verify that codes adhere to current coding guidelines and regulations, minimizing the risk of billing errors and audits.
-
Automated Data Entry:AI can extract relevant information from electronic health records (EHRs) and automatically populate coding fields, reducing manual data entry time.
-
Workflow Optimization:AI can analyze coding workflows and suggest improvements to streamline processes, increasing coder productivity and throughput.
While AI will continue to evolve and improve the efficiency and accuracy of medical coding and billing, human coders remain vital for handling complex, nuanced cases, making ethical decisions, and ensuring quality control. AI will enhance productivity, but the skills and judgment of medical coders will always be essential in delivering high-quality, accurate coding and billing in the healthcare system.