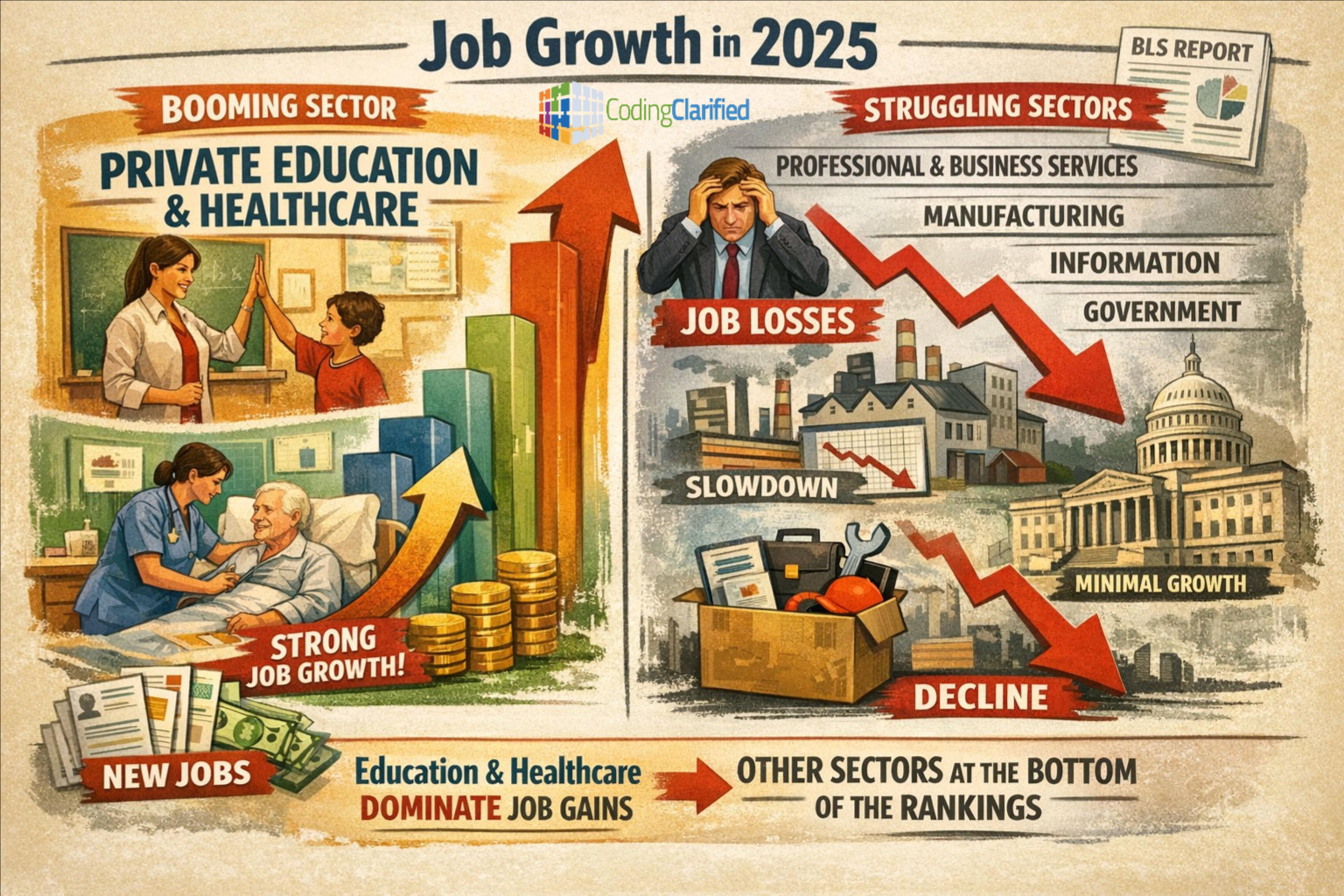
Recent reporting on the U.S. jobs picture
Coverage of the January 9, 2026, jobs report focused mainly on overall weak U.S. job growth for 2025, noting that the total number of jobs added was much lower than usual, and the broader job market has been sluggish entering 2026. Analysts described most industries as being in a “hiring recession.”
The discussion highlighted that certain sectors—especially health care and social services and leisure/hospitality—accounted for most of the job gains, even while many other industries struggled.
Healthcare and education jobs are relatively bright spots
According to the Bureau of Labor Statistics’ projection data , the healthcare and social assistance sector is projected to grow faster than any other major industry through the next decade. It is expected to add the most new jobs among all sectors through around 2034, driven largely by an aging population and expanding demand for care services.
BLS occupational forecasts also show many health care–related roles (like nurse practitioners, physician assistants, home health aides, etc.) ranked among the fastest-growing occupations in the job market.
Education jobs, especially in health-related teaching roles (e.g., health specialties teachers), also appear on lists of sectors with above-average growth.
Why do these sectors show strength?
Healthcare demand is driven by demographic trends (notably the aging U.S. population needing more medical and long-term care). This underpins ongoing hiring in hospitals, outpatient services, home health, and related support roles.
Education (especially postsecondary/health specialties teaching) benefits from broader workforce needs, including training new professionals for these growing fields.
In the context of a slow overall labor market, these sectors stand out because they are rooted in fundamental social needs (healthcare for a growing elderly cohort and education for workforce development) that are less tied to short-term economic cycles.
Overall job growth context
Despite these areas of relative strength, total U.S. job growth remains weak entering 2026, with only modest gains and many sectors (like manufacturing, construction, and some services) showing slow or negative trends.
Job gains are heavily concentrated, meaning healthcare and related education services account for a disproportionate share of job creation while other industries lag.
Private education and healthcare jobs have been among the most resilient and fastest-growing areas in the U.S. labor market.
Healthcare, especially, is a leading growth engine, and many related occupations and educational roles are projected to continue expanding through 2026 and beyond.
However, overall labor market growth remains subdued outside those sectors.
It directly relates to medical coding
When CNN (and the BLS data they reference) show private education and healthcare as one of the strongest job-growth sectors going into 2026, medical coding is part of that growth pipeline.
Here’s how it connects:
Healthcare expansion automatically increases the need for:
-
Medical coders
-
Risk adjustment (HCC) coders
-
Outpatient and physician office coders
-
Facility coders
-
Compliance and audit coders
Every patient visit, procedure, surgery, test, and diagnosis must be coded for:
-
Insurance reimbursement
-
Medicare and Medicaid billing
-
Risk adjustment programs
-
Quality reporting
-
Value-based care models
More patients = more claims = more coding.
Why private education matters for medical coding
Private education growth includes:
-
Career schools
-
Certification programs
-
Online healthcare training programs
-
Professional certification prep
Medical coding programs fall directly into this category.
As healthcare systems expand, they need:
-
More coders
-
More billers
-
More auditors
-
More compliance specialists
Which creates demand for:
-
CPC training programs
-
Credentialing programs
-
Continuing education (CEUs)
-
Specialty coding programs
This is exactly the space Coding Clarified operates in.
What this means for coders in 2026 and beyond
Healthcare is one of the most recession-resistant industries because:
-
People always need care
-
Medicare enrollment is growing rapidly
-
Chronic disease management is increasing
-
Telehealth and outpatient services continue expanding
All of those trends increase coding volume.
That’s why even when other industries slow, healthcare keeps hiring—and coders are essential infrastructure.
A recent job growth graph showing strength in private education and healthcare is a strong signal for:
-
Job stability in medical coding
-
Continued hiring demand
-
Long-term career growth
-
Expansion of certification and training programs
Medical coding sits right at the intersection of those two growing sectors.
Here’s a comprehensive breakdown
How U.S. job growth projections relate specifically to medical coding—including current data, future demand, trends, and what it means for careers in 2026 and beyond.
Healthcare drives overall job growth
Why this matters: The healthcare and social assistance sector is the largest source of new jobs in the U.S. economy, projected to add millions of jobs over the next decade, and it’s the main driver of total employment growth.
This broad healthcare expansion ripples into administrative and technical roles like medical coding, billing, and health information.
Medical coding falls under the health information roles
Medical coders are usually classified within the “medical records and health information technicians” occupation group.
This category includes professionals who:
-
Assign standardized codes to diagnoses and procedures
-
Translate clinical documentation into code sets used for billing and analytics
-
Work with electronic health record (EHR) systems
-
Help ensure accurate healthcare reimbursement and compliance
Job growth projections for coding-related occupations
Medical records and health information technicians
Projected growth: 7% from 2024 to 2034—much faster than the average for all occupations.
Annual openings: Around 14,000+ openings per year, partly from demand and retirements.
This group includes coders and is a key source of future medical coding jobs.
Health information technologists and medical registrars
This related but higher-level category (often involving data analytics, IT systems, and registry work) is projected to grow 15% from 2024 to 2034, again much faster than average.
While not purely coding roles, many professionals in this field need strong coding knowledge and can move into coding, auditing, analytics, or health data leadership roles.
Medical billers and coders (industry data)
Multiple career outlook sources estimate that medical billing and coding jobs will grow around 8–9% over the 2020s, faster than average overall.
This growth reflects the increasing volume of healthcare services, telemedicine expansion, and the complexity of reimbursement systems.
What’s driving demand for coders?
Healthcare growth
An aging population and rising prevalence of chronic conditions mean more healthcare visits and services, all needing coding.
Telehealth and new services
Remote/virtual care has become a standard part of healthcare delivery and has added new coding categories and requirements, which increases work for coders.
Health data and RCM trends
Revenue cycle management (RCM) outsourcing, compliance needs, and expanded data reporting functions contribute to the demand for skilled coding professionals.
Market size and growth trends
External industry research projects significant growth in the medical coding market itself:
-
The U.S. medical coding market is estimated to grow to over $51 billion by 2033, with about 10% annual compound growth.
-
Another forecast estimates billing and coding sector revenue will double from 2024 to 2033.
This reflects not just job openings but demand for coding services, tools, platforms, and outsourcing—all of which expand career opportunities.
Career trends in 2026 and beyond
Based on data and industry insights, here are the key trends impacting coding careers:
Emerging roles and skills
AI-assisted coding helps automate routine tasks but still requires human oversight.
Hierarchy Condition Category (HCC) and risk-adjustment coding are in higher demand as payers emphasize value-based care.
Flexible work models
Remote and hybrid coding positions are increasingly common, expanding opportunities nationally.
Certifications matter
Credentials like CPC, CCS, CPMA, RHIT, etc., remain critical for advancement and higher pay.
What this means for you
Medical coding is positioned for continued growth and stability:
-
Growth rates for coding and health information roles are consistently higher than average compared to most occupations.
-
Healthcare job expansion broadly supports coding demand, even when other industries slow.
-
Technological shifts and telehealth are creating new coding needs and increasing specialization opportunities.
Healthcare job growth is strong and a major driver of total employment increases.
Medical coding jobs (within health information tech) are projected to grow faster than average.
Demand is fueled by aging populations, telehealth, data needs, and revenue cycle complexity.
Market reports also show robust growth in the coding services sector itself.
Here’s the latest salary, job growth, and where medical coding and related health-information careers are growing the most strongly.
Salary and pay expectations for medical coders
Typical earnings nationally
The median annual wage for medical records and health information specialists (which includes medical coders) was about $50,250 in 2024, similar to the wage for coders reported by several career sources.
Many survey reports show a median of around $50,000–$53,000 per year, with variations based on experience, certifications, and location.
Top earners (the highest 10%) can make more than $75,000 per year, especially with strong skills, certifications, or in high-pay markets.
Impact of education and credentials
Coders with associate or bachelor’s degrees and professional certifications often earn more than entry-level coders. Some data show median salaries around $59,000–$60,000 with more formal training.
Salary can rise further with advanced credentials, experience, and specialization, such as HCC risk adjustment, auditing, or compliance coding.
Job growth and demand (2024–2034)
Growth projections
The Bureau of Labor Statistics projects employment of medical records specialists (including coders) to grow about 7% from 2024 to 2034, which is faster than the average for all occupations. This translates to roughly 14,000 job openings per year on average.
Other industry sources estimate similar or slightly stronger growth for medical billing and coding roles—8%–9% growth and ~16,000+ openings annually over the next decade.
Why growth is happening
Healthcare utilization continues to rise due to demographic trends and expanded services, generating ongoing demand for coding expertise.
Even with AI and automation tools evolving, coders still drive complex documentation, compliance, and reimbursement accuracy.
Higher-level health information jobs
If you’re thinking beyond basic coding, there are higher-paying roles in health information management:
Health information technologists and medical registrars
Median annual wage was around $67,310 in 2024.
Projected to grow 15% from 2024 to 2034, much faster than average.
These roles often involve data analysis, system implementation, or clinical database oversight—and many coders advance into these positions over time.
Which states/regions pay more or have higher demand
While detailed state-by-state BLS data for coders isn’t always published in summary results, current trends show:
High-pay or high-demand markets
States like California, New York, Maryland, and the District of Columbia often have higher salary ranges for coders and other health information roles.
Large healthcare hubs such as Texas and Florida also show strong employment opportunities, even if salaries are somewhat lower than in high-cost states.
In health information technologist jobs, California’s average wages for these roles can exceed $100,000/year in some industries.
Why these areas stand out
States with large hospital networks, outpatient centers, insurance firms, and tech-health ecosystems tend to invest more in health data and coding expertise.
High cost-of-living regions often offer higher nominal wages to attract skilled professionals.
Career flexibility and remote work
Remote coding jobs
Many employers now offer remote medical coding positions, which increases job flexibility and access to roles outside your immediate geographic area.
Growth with technology
While AI tools assist routine tasks, experts will still be needed to handle complex cases, quality assurance, compliance, audits, and payer-specific requirements.
What this means for 2026–2030
Medical coding is a solid, growing career because:
-
The healthcare sector is expanding faster than average overall.
-
Coders and medical records specialists are projected to see job growth faster than average.
-
Salaries are competitive and can be significantly higher with specialization and certification.
-
Remote and hybrid work options are broadening job access.
-
Higher-level health information roles offer advanced career pathways with stronger growth and pay.
Here’s a clear, practical breakdown of the certifications
Based on employer demand trends, hiring patterns, and advancement pathways these credentials have the most improve earning potential, job access, and long-term career growth in medical coding for 2026 and beyond.
The certifications that matter most for pay and hiring
CPC (Certified Professional Coder) — AAPC
The industry gold standard
This is still the most requested credential in job postings.
Best for:
-
Physician office coding
-
Outpatient coding
-
Remote coding roles
-
Entry-to-mid level coders
Why it boosts pay:
-
Required or preferred by most employers
-
Unlocks remote work eligibility
-
Required for most payer contracts and RCM vendors
Typical impact:
-
Entry coders often start in the $45,000–$55,000 range
-
With experience: $55,000–$70,000+
-
With specialization: $70,000–$85,000+
CCS (Certified Coding Specialist) — AHIMA
Hospital and inpatient coding powerhouse
Highly valued by hospital systems and large healthcare networks.
Best for:
-
Inpatient coding
-
Facility coding
-
Trauma and surgical cases
-
DRG and MS-DRG environments
Why it boosts pay:
-
Hospitals pay more for CCS than CPC
-
Often required for inpatient roles
-
Strong demand due to staffing shortages
Typical impact:
-
Hospital coders commonly earn $60,000–$80,000+
-
Senior inpatient coders: $80,000–$95,000+
CPMA (Certified Professional Medical Auditor) — AAPC
One of the highest-paying credentials
This moves you into auditing, compliance, and revenue integrity.
Best for:
-
Compliance auditing
-
Risk and quality reviews
-
Internal payer audits
-
Provider education
Why it boosts pay:
-
Audit roles pay significantly more than production coding
-
Fewer qualified professionals than coding roles
-
High demand due to payer scrutiny
Typical impact:
-
Audit roles commonly pay $75,000–$100,000+
-
Senior auditors can exceed $110,000
CRC (Certified Risk Adjustment Coder) — AAPC
Exploding demand with Medicare Advantage growth
Risk adjustment and HCC coding is one of the fastest-growing niches.
Best for:
- Medicare Advantage
- Value-based care
- Population health
- Chronic condition management
Why it boosts pay:
- MA enrollment growing rapidly
- Payers heavily invest in HCC accuracy
- Outsourced vendors pay premium rates
Typical impact:
- Risk coders commonly earn $70,000–$95,000
- Project-based coders can earn even more
COC (Certified Outpatient Coder) — AAPC
Facility outpatient specializationGreat for hospital outpatient departments and surgery centers.
Best for:
- ASC coding
- Hospital outpatient
- Observation services
- Same-day surgery
Typical impact:
- $60,000–$80,000 range with experience
RHIT / RHIA — AHIMA
Health information leadership trackThese move you beyond coding into health data, systems, and management.
Best for:
- HIM management
- Data analytics
- Compliance leadership
- Registry and reporting
Why do they boost pay:
- Qualify for management roles
- Required for many leadership positions
Typical impact:
- RHIT: $60,000–$80,000
- RHIA: $80,000–$110,000+
The best certification path for maximum earnings
Here’s the most common high-earning progression:
Path 1: Coding to audit/compliance
CPC → CPMA → Compliance/Audit Director
This is the highest-earning long-term path.
Path 2: Coding to risk adjustment
CPC → CRC → Risk Adjustment Lead
Very strong demand and remote flexibility.
Path 3: Coding to hospital leadership
CPC or CCS → RHIT → RHIA
Leads to HIM management and executive roles.
Certifications that employers are requesting most in 2026 job listings
Based on hiring patterns:
-
CPC
-
CCS
-
CRC
-
CPMA
-
COC
These appear most frequently in job postings for:
-
Remote roles
-
Contract projects
-
Compliance teams
-
Hospital systems
-
Medicare Advantage plans
What this means for coders in 2026 and beyond
Healthcare hiring growth plus regulatory complexity means:
-
More audits
-
More payer reviews
-
More compliance oversight
-
More risk adjustment scrutiny
-
More revenue protection initiatives
All of those require certified coders.
AI tools increase productivity but do not replace certified professionals—they increase the need for auditors, validators, and compliance experts.
Medical coding remains a strong, stable, and scalable career path because it sits at the center of healthcare reimbursement.
The certifications that most increase income and job security are:
-
CPC
-
CCS
-
CPMA
-
CRC
-
RHIT/RHIA
Coders who specialize and credential strategically will be positioned for the strongest job growth, highest pay, and best remote opportunities through 2030 and beyond.
This is the same pathway most successful coders use to move from certification → employment → specialization → higher income.
CPC career roadmap (2026–2027)
Phase 1 — CPC certification (Months 0–6)
Goal: Pass the CPC exam and become job-ready.
Coding Clarified can train you for the CPC, as we are an AAPC-approved education provider. You may even qualify for a scholarship/grant!
Coding Clarified Medical Coding course includes the following:
80-clock-hour course
100% remote studies
Access to the AAPC online medical coding class
CPT, ICD10, HCPC and Textbook
Instructor video/audio files to implement notes into your books
1:1 time with instructor as needed
Professionally written resume (Upon completion of internship)
AAPC Membership (Assigned at completion of course)
CPC Exam Voucher x2 (Assigned at completion of course)
Job placement assistance/resources (Once certified or completed with Internship)
Online HCC Internship (Once completed with Practicode)
Practicode (Upon becoming certified as CPC)
CPC Practice Exam Bundle x3 (Upon completion of course)
CPC Study Guide (Electronic)
CPC Exam Online Review (Upon completion of the course)
Coding Clarified AAPC CPC WIOA Scholarships/Grant
CPC study calendar (12-week certification plan)
Week 1–2
Medical terminology, anatomy, ICD-10-CM guidelines
Week 3–4
Integumentary and musculoskeletal CPT coding
Week 5–6
Digestive, respiratory, cardiovascular coding
Week 7–8
Nervous system, radiology, pathology, medicine
Week 9
E/M guidelines and MDM
Week 10
Modifiers and compliance
Week 11
Full practice exams
Week 12
Final review and exam readiness
Daily:
-
2 hours study
-
30 practice questions
-
10 ICD-10 diagnoses
-
10 CPT scenarios
Step 1: Core skills to master
A strong CPC candidate must be confident in:
-
CPT coding (E/M, surgery, modifiers)
-
ICD-10-CM guidelines
-
HCPCS Level II
-
Compliance and documentation
-
Medical terminology and anatomy
Employer expectation:
They assume a CPC understands:
-
Payer rules
-
CMS vs AMA CPT guidelines
-
Modifier logic
-
Medical necessity
Step 2: Pass the CPC exam
Exam essentials:
-
100 questions
-
4 hours
-
Open book (CPT, ICD-10-CM, HCPCS)
-
Heavy focus on:
-
E/M
-
Surgery
-
Modifiers
-
Compliance
-
CPC success toolkit for 2026–2027—designed for certification, hiring, and career growth
This is structured the same way employers, recruiters, and audit teams evaluate coders.
CPC 2026 success toolkit
Certification. Hiring. Career growth.
Part 1 — CPC study strategy (2026 exam focused)
What the CPC exam tests most heavily
You are not tested equally on every section. The exam is heavily weighted toward:
-
CPT surgery (largest section)
-
E/M (office visits, hospital, ED)
-
Modifiers
-
ICD-10-CM guidelines
-
Compliance and regulations
-
HCPCS Level II
If you master those, you pass.
The CPC study framework (12–16 weeks)
Phase 1 — Foundation (Weeks 1–4)
Focus:
-
Medical terminology
-
Anatomy
-
ICD-10-CM guidelines
-
CPT structure
Daily goals:
-
1 body system per day
-
20–30 ICD-10 practice cases
-
Read CPT guidelines before each section
Key areas:
-
Neoplasms
-
Diabetes
-
Hypertension
-
Injuries
-
External cause codes
-
Laterality
-
Sequela
Phase 2 — CPT mastery (Weeks 5–9)
This is where most people fail.
Study order:
-
Integumentary
-
Musculoskeletal
-
Digestive
-
Respiratory
-
Cardiovascular
-
Nervous system
Daily goals:
-
20–40 CPT cases
-
Surgical approach logic
-
Anatomy correlation
Key concepts:
-
Bundling
-
Global periods
-
Separate procedures
-
Add-on codes
-
Unlisted codes
Phase 3 — E/M + modifiers (Weeks 10–12)
This section is high scoring and high impact.
Master:
-
2025–2026 E/M guidelines
-
Medical decision making
-
Time-based coding
-
Modifier 25
-
Modifier 59
-
Modifier 51
-
Modifier 26
-
Modifier TC
Phase 4 — Compliance and final review (Weeks 13–16)
Know:
-
OIG
-
False Claims Act
-
HIPAA
-
NCCI edits
-
LCD vs NCD
-
ABNs
-
Incident-to
Practice:
-
Full-length exams
-
Timed tests
-
Book navigation speed
Exam day strategy
-
Tab all code books
-
Highlight guidelines
-
Use a time strategy:
-
50 questions in first 90 minutes
-
Remaining 50 in next 90 minutes
-
60 minutes review
-
Once passed:
You earn CPC-A (Apprentice) status if you lack experience.
Phase 2 — Removing CPC-A (Months 6–12)
Goal: Remove apprentice status and become fully credentialed.
You need:
-
2 years of experience OR
-
1 year experience + approved practicum
-
Or approved training + Practicode
Common paths:
Path A — Practicode
-
Simulated real-world cases
-
Removes 1 year of apprentice status
Path B — Employer entry role
-
Billing + coding hybrid
-
Charge entry
-
Prior auth
-
Coding support
Many employers hire CPC-A if you show:
-
Strong CPT knowledge
-
Compliance awareness
-
Production accuracy
Phase 3 — First coding job (Months 9–15)
Goal: Land your first production coding role.
Typical entry roles:
-
Physician office coder
-
RCM coding specialist
-
Outpatient coding
-
Billing and coding analyst
-
Coding support specialist
Expected salary range:
-
$45,000–$55,000
-
Remote eligible after training period at many employers
Phase 4 — Specialization (Months 12–18)
Goal: Increase pay and job security.
Once you have:
-
6–12 months of production coding
-
Proven accuracy and productivity
You can move into:
High-demand CPC specializations
Risk adjustment/HCC
-
Medicare Advantage
-
Chronic condition coding
-
Chart reviews
-
Remote project work
Pay range: $70,000–$95,000
Outpatient facility coding
-
Hospital outpatient departments
-
Same-day surgery
-
Observation services
Pay range: $60,000–$80,000
Compliance and internal audits
-
Coding quality
-
Provider education
-
Denial prevention
Pay range: $70,000–$90,000
What employers want from CPC coders in 2026
Hiring managers consistently look for:
-
CPC certification
-
Strong modifier knowledge
-
Compliance awareness
-
Productivity discipline
-
Audit readiness
-
Remote work capability
They do not expect:
-
Inpatient DRG knowledge
-
CCS-level facility coding
That’s a different track.
The fastest CPC career path to $75K+
Most common successful path:
Month 0–6 → CPC certified
Month 6–12 → Entry coding role
Month 12–18 → Risk or outpatient specialization
Month 18–24 → Senior coder/auditor
This is how many coders reach:
-
$70K–$85K within 2 years
-
$90K+ within 3–4 years
The CPC is still the strongest single credential for:
-
Job access
-
Remote work
-
Career mobility
-
Specialization
-
Long-term stability
Healthcare hiring growth plus reimbursement complexity means CPC coders will remain in demand through 2030 and beyond.
Part 2 — CPC resume template (hiring-ready)
This format passes both recruiter screening and ATS software.
Name, CPC-A
City, State | Remote eligible
Email | Phone | LinkedIn
Professional summary
Certified Professional Coder (CPC-A) with strong knowledge of CPT, ICD-10-CM, and HCPCS Level II coding. Trained in outpatient and physician-based coding with a focus on documentation accuracy, compliance, and revenue integrity. Detail-oriented and audit-ready with strong proficiency in EHR systems and payer guidelines.
Certifications
Certified Professional Coder (CPC-A) — AAPC
Expected apprentice removal: [Month/Year]
Technical skills
-
CPT, ICD-10-CM, HCPCS Level II
-
Modifier application (25, 59, 51, 26, TC)
-
E/M coding (2025–2026 guidelines)
-
Surgical coding
-
Compliance and audit readiness
-
Medical necessity validation
-
LCD/NCD research
-
Denial prevention
Coding experience
Medical coding practicum/Practicode
-
Assigned diagnosis and procedure codes using ICD-10-CM and CPT
-
Reviewed clinical documentation for accuracy and completeness
-
Applied payer-specific coding rules
-
Ensured compliance with CMS and AMA guidelines
-
Maintained 95%+ coding accuracy
Software
Epic
Cerner
Athena
eClinicalWorks
NextGen
3M Encoder
Optum Encoder
Education
Medical coding program
School name
Part 3 — Employers that hire CPC-A and remote coders
These employers consistently hire new CPCs and train:
National healthcare systems
-
UnitedHealth Group/Optum
-
Humana
-
Aetna/CVS Health
-
Centene
-
Cigna
-
Elevance Health (Anthem)
-
Kaiser Permanente
-
HCA Healthcare
-
CommonSpirit
-
Tenet Healthcare
Coding and RCM companies
-
nThrive
-
GeBBS Healthcare
-
CSI Companies
-
AGS Health
-
Ensemble Health
-
Change Healthcare
-
Conifer Health
Risk adjustment vendors
-
Cotiviti
-
Signify Health
-
Optum Risk
-
Ciox Health
-
Episource
-
Advantmed
-
Reveleer
-
Inovalon
Where to apply
-
Company career pages
-
LinkedIn Jobs
-
Indeed
-
AAPC job board
-
RCM vendor sites
Search terms:
-
CPC-A
-
Medical Coder I
-
Coding Specialist
-
Coding Analyst
-
Risk Adjustment Coder
-
Outpatient Coder
Part 4 — Fast-track CPC career plan
Month 0–6
CPC Certification
Month 6–12
Entry coding role or practicum
Month 12–18
Specialization (risk, outpatient, compliance)
Month 18–24
Senior coder or auditor
Income path:
Year 1: $45K–$55K
Year 2: $60K–$75K
Year 3+: $75K–$95K
The CPC is the strongest single credential in the healthcare revenue cycle.
Healthcare hiring growth, payer complexity, Medicare expansion, and compliance scrutiny mean certified coders are essential infrastructure.
Coders who follow this roadmap position themselves for:
-
Remote work
-
Career stability
-
Long-term income growth
-
Leadership roles
CPC interview prep guide (hiring manager ready)
What hiring managers are actually evaluating
They are not just testing coding knowledge. They are evaluating:
-
Accuracy mindset
-
Compliance awareness
-
Productivity discipline
-
Documentation integrity
-
Audit readiness
-
Trainability
They want to know:
Can we trust you with our revenue?
The 10 most common CPC interview questions
Walk me through how you code a chart.
Strong answer:
I start by reviewing the provider documentation for completeness and medical necessity. I identify the chief complaint, assessment, plan, and procedures. I assign ICD-10-CM codes following official guidelines and apply CPT codes using CPT guidelines and payer rules. I validate modifiers, check NCCI edits, and ensure compliance with LCD and NCD policies.
How do you ensure coding accuracy?
Strong answer:
I follow official guidelines, payer policies, and CPT instructions. I use encoder tools and verify against code books. I audit my own work and track accuracy metrics.
What do you do if the documentation is unclear?
Strong answer:
I query the provider for clarification following compliance standards. I never assume or upcode.
What modifiers do you use most often?
Be prepared to explain:
-
25
-
59
-
51
-
26
-
TC
-
57
How do you handle productivity goals?
Strong answer:
I focus on accuracy first, then efficiency. I build speed through repetition and workflow discipline.
What is medical necessity?
Strong answer:
Services must be reasonable and necessary based on diagnosis, documentation, and payer policy.
What is NCCI?
Strong answer:
The National Correct Coding Initiative prevents improper unbundling and duplicate billing.
How do you stay current?
Strong answer:
I review CPT and ICD-10 updates annually, attend CEUs, and follow CMS guidance.
What EHR systems have you used?
Have a list ready:
Epic, Cerner, Athena, NextGen, eClinicalWorks, etc.
Why should we hire you?
Strong answer:
I bring strong coding fundamentals, compliance awareness, audit readiness, and a commitment to accuracy and integrity.
CPC portfolio template (this gets you hired)
A portfolio separates you from 90 percent of candidates.
Section 1 — Certification
-
CPC certificate
-
Transcript
-
CEUs
-
Practicum completion
Section 2 — Coding samples (de-identified)
Include:
-
5 outpatient visit charts
-
5 surgical cases
-
5 modifier cases
-
5 diagnosis-heavy cases
Each should show:
-
ICD-10-CM codes
-
CPT codes
-
Modifiers
-
Rationale
Section 3 — Compliance knowledge
Include:
-
Medical necessity example
-
NCCI edit example
-
LCD research example
-
Provider query example
Section 4 — Productivity tracking
Show:
-
Accuracy rate
-
Charts per hour
-
Turnaround time
Section 5 — Software
List:
-
EHRs
-
Encoders
-
Billing systems
Job application tracker (use this format)
Company
Role
Recruiter
Date applied
Status
Follow-up date
Notes
Optum
Coding Specialist I
Jane Doe
3/5/26
Interview
3/12/26
Remote
Humana
CPC-A Coder
John Smith
3/7/26
Screening
3/14/26
Risk
Apply to 10–15 jobs per week.
Follow up after 7 days.
First 90 days on the job success plan
Days 1–30: Accuracy phase
Your only goal is accuracy.
-
Learn payer policies
-
Learn EHR workflows
-
Understand escalation paths
-
Hit 95% accuracy
Do not rush.
Days 31–60: Speed phase
Now build productivity.
-
Improve navigation speed
-
Build shortcuts
-
Master top 20 codes
-
Reduce chart time
Target:
85–90% of productivity goal
Days 61–90: Excellence phase
Now stand out.
-
Volunteer for audits
-
Offer provider education
-
Track denial trends
-
Request specialty training
This is how you get promoted.
Your 24-month CPC career map
Month 0–6
CPC certification
Month 6–12
Entry coding role
Month 12–18
Specialization (risk, outpatient, compliance)
Month 18–24
Senior coder or auditor
Income trajectory:
Year 1: $45K–$55K
Year 2: $60K–$75K
Year 3: $75K–$95K
The CPC is not just a certification.
It is a professional license to protect healthcare revenue.
Healthcare growth, Medicare expansion, value-based care, audits, and compliance scrutiny guarantee long-term demand for certified coders.
Coders who follow this framework build:
-
Job security
-
Remote flexibility
-
Career mobility
-
Long-term income growth
Absolutely. Below is your complete CPC professional launch package—ready to use for students, job seekers, and career changers.
This is written to employer expectations and recruiter standards for 2026 and beyond.
CPC interview script (rehearsal version)
Use this to practice and build confidence.
Opening introduction (tell me about yourself)
I am a Certified Professional Coder with strong training in CPT, ICD-10-CM, and HCPCS Level II coding. My background includes outpatient and physician-based coding with a focus on documentation accuracy, compliance, and reimbursement integrity. I am detail-oriented, audit-ready, and committed to maintaining high accuracy while meeting productivity standards.
How do you code a chart?
I begin by reviewing the provider documentation for completeness and medical necessity. I identify the chief complaint, assessment, plan, and procedures performed. I assign ICD-10-CM codes following official guidelines, then apply CPT codes using CPT instructions and payer rules. I validate modifiers, check NCCI edits, and confirm LCD and NCD policies when applicable.
How do you ensure accuracy?
I follow official coding guidelines, payer policies, and CPT instructions. I use encoder tools and verify codes against code books. I audit my own work, track accuracy metrics, and seek clarification when documentation is unclear.
What do you do if documentation is missing?
I submit a compliant provider query following organizational and regulatory standards. I never assume or infer diagnoses or procedures.
What modifiers do you use most often?
Modifier 25 for significant E/M services, Modifier 59 for distinct procedural services, Modifier 51 for multiple procedures, Modifier 26 for professional components, and Modifier TC for technical components.
What is medical necessity?
Medical necessity means that services are reasonable and necessary based on the patient’s condition, clinical documentation, and payer policy.
What is NCCI?
The National Correct Coding Initiative prevents improper unbundling and duplicate billing.
How do you handle productivity goals?
I prioritize accuracy first. Once accuracy is established, I build speed through workflow optimization, repetition, and familiarity with high-volume codes.
Why should we hire you?
I bring strong coding fundamentals, compliance awareness, audit readiness, and a commitment to protecting healthcare revenue through accurate documentation and coding.
Recruiter outreach message template
Use on LinkedIn or email.
Hello [Recruiter Name],
I am a Certified Professional Coder (CPC) seeking an opportunity in outpatient or physician-based coding. I have strong experience with CPT, ICD-10-CM, modifiers, and payer compliance. I am particularly interested in roles with [Company Name] due to your strong reputation in healthcare delivery and revenue integrity.
I would welcome the opportunity to discuss how my skills can support your coding and compliance goals.
Thank you for your time and consideration,
[Your Name], CPC
LinkedIn profile that attracts recruiters
Headline
Certified Professional Coder (CPC) | Outpatient and Physician Coding | Revenue Cycle | Compliance | Remote Ready
About section
Certified Professional Coder with strong expertise in CPT, ICD-10-CM, and HCPCS Level II coding. Experienced in outpatient and physician-based coding with a focus on documentation accuracy, medical necessity validation, and payer compliance. Known for high accuracy, audit readiness, and strong productivity discipline. Seeking opportunities in physician, outpatient, risk adjustment, or compliance coding environments.
Skills
-
CPT coding
-
ICD-10-CM
-
HCPCS Level II
-
Modifier application
-
E/M guidelines
-
Medical necessity
-
NCCI edits
-
Compliance auditing
-
Revenue cycle management
-
Epic, Cerner, Athena, NextGen
CPC portfolio checklist
Use this for job interviews.
-
CPC certificate
-
Coding transcript
-
Practicum or Practicode completion
-
20 de-identified coding cases
-
Modifier examples
-
Compliance examples
-
Accuracy metrics
-
Software proficiency list
Job search strategy
Apply to:
- Medical Coder I
- Coding Specialist
-
Outpatient Coder
-
Physician Coder
-
Risk Adjustment Coder
-
RCM Analyst
Apply to 10–15 jobs per week.
Follow up after 7 days.
Track applications in a spreadsheet
First 90 days on the job
Days 1–30
Accuracy, training, compliance mastery
Days 31–60
Speed, workflow efficiency, productivity
Days 61–90
Excellence, audits, specialty training
Final takeaway
The CPC credential is a direct gateway into healthcare revenue cycle careers.
Healthcare growth, Medicare expansion, compliance enforcement, and audit activity guarantee long-term demand for certified coders.
Coders who follow this roadmap build:
-
Career stability
-
Remote flexibility
-
Professional mobility
- Long-term income growth
BLS THE EMPLOYMENT SITUATION — DECEMBER 2025