Overview: What is a Brain Aneurysm?
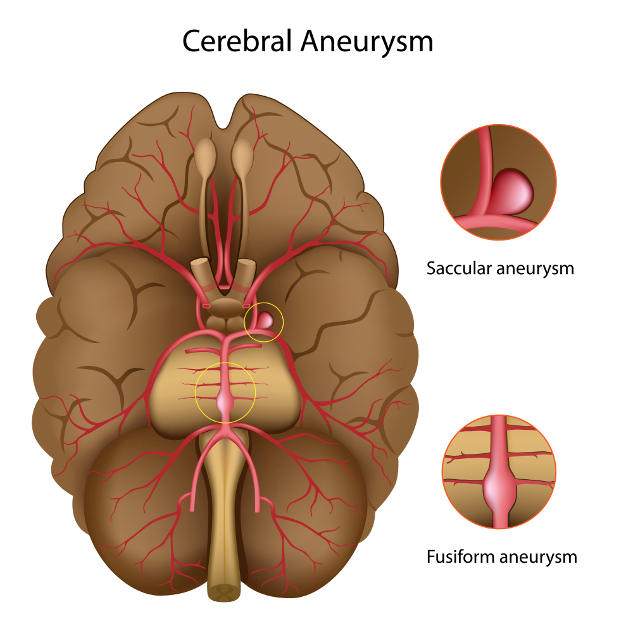
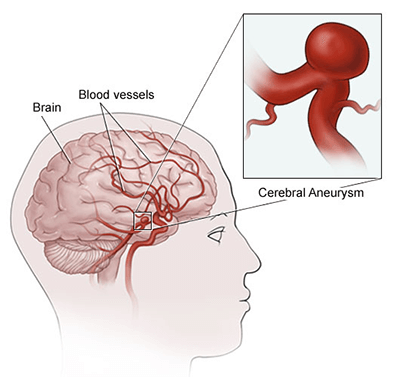
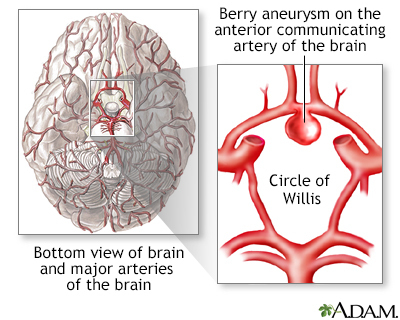
A brain aneurysm (also known as a cerebral or intracranial aneurysm) is a weakened area in the wall of a blood vessel in the brain that bulges or balloons out. It most commonly occurs at arterial branch points (e.g., at the base of the brain and the Circle of Willis) and, if ruptured, may cause a subarachnoid hemorrhage or other intracranial bleeding.
From a medical coding brain aneurysm perspective, two major distinctions are essential:
-
Non-ruptured aneurysm (aneurysm present but no bleed)
-
Ruptured aneurysm (aneurysm has caused bleeding, most often subarachnoid hemorrhage (SAH))
Key Diagnosis Codes (ICD-10-CM)
Non-ruptured cerebral aneurysm
-
Use I67.1: Cerebral aneurysm, nonruptured.
-
Includes: “cerebral aneurysm NOS”, “internal carotid artery aneurysm, intracranial portion” among others.
-
Excludes (Type 1): congenital cerebral aneurysm (Q28.–) and ruptured cerebral aneurysm (I60.x) – meaning these conditions are coded separately.
-
-
Documentation must confirm that the aneurysm is non-ruptured, including imaging findings, location, size, treatment plan, etc.
Ruptured cerebral aneurysm
-
Rupture typically leads to a non-traumatic subarachnoid hemorrhage (SAH). Use codes in the I60.00–I60.9 range.
-
The specific code depends on artery location, side (laterality), etc.
-
-
Be sure documentation clearly attributes the hemorrhage to the aneurysm rupture (non-traumatic).
History of aneurysm
-
For a treated/resolved aneurysm (no longer active), code Z86.79: Personal history of other diseases of the circulatory system, when it’s specifically documented as a history of brain aneurysm.
-
Important: Don’t code I67.1 for an aneurysm that has been definitively treated/resolved and is no longer present.
Key Procedure Coding Guidelines (ICD-10-PCS)
When coding inpatient procedures for aneurysm treatment, the correct root operation (3rd character in PCS) hinges on the objective of the procedure.
-
For most aneurysm repairs (e.g., endovascular coiling/embolization or surgical clipping) the operation is Restriction, not Occlusion — because the goal is narrowing or excluding the aneurysm from the lumen of the artery while maintaining flow, not necessarily completely closing the parent vessel.
-
Example: Embolization of a cerebral aneurysm = root operation Restriction (supported by guideline B3.12).
-
If the procedure’s objective is complete closure of the vessel (rare for aneurysm unless parent vessel sacrifice is performed), then root operation would be Occlusion.
Remember:
-
Review the approach, device, and body part in the PCS code selection.
-
Confirm documentation mentions: “excluded aneurysm from circulation”, “coil placed into aneurysm sac”, “clip applied to aneurysm neck with parent vessel patent”, etc.
Documentation & Coding Tips to Avoid Pitfalls
-
Ensure rupture status (non-ruptured vs rupture with SAH) is clearly documented. If not, you risk selecting the wrong diagnosis code (and the DRG may differ).
-
For non-ruptured aneurysms: include location (which artery, side), size of aneurysm, imaging modality (CTA/MRA/Angiogram), whether treatment plan is in place or observation. Good documentation example: “6 mm saccular aneurysm at right MCA bifurcation, non-ruptured, confirmed by CTA.”
-
For ruptured aneurysms: documentation should reflect imaging (CT showing SAH), origin of hemorrhage (aneurysm rupture) and specify artery and side if known. Avoid unspecified when laterality is given.
-
For treatment/procedure coding: coders must read operative reports carefully to determine objective (restriction vs occlusion), method (clipping vs coiling vs flow-diverter), device used, approach, and body part.
-
If documentation is vague (e.g., “aneurysm treated endovascularly”), query the physician for specifics: was the parent vessel sacrificed (occlusion) or was the aneurysm sac excluded while maintaining parent flow (restriction)?
-
For follow-up visits after aneurysm treatment, or surveillance imaging when aneurysm remains untreated/observed: check if aneurysm is still present vs history. Use Z-codes for history where appropriate.
-
Avoid miscoding an untreated non-ruptured aneurysm as history only — this could mask risk and affect care management and coding accuracy.
Sequencing & Reporting Considerations
-
For inpatient admissions: if a patient presents with SAH due to aneurysm rupture, the SAH code (I60.x) is reported as principal diagnosis (since it drives the admission and treatment). The aneurysm code may be an additional diagnosis if documented and treated.
-
For a non-ruptured aneurysm admitted for treatment (e.g., clipping/embolization), the aneurysm code I67.1 would be principal diagnosis because it’s the reason for the admission.
-
Multiple aneurysms? Document each location and status; code each as appropriate based on rupture status.
-
For history of treated aneurysm and no current aneurysm: use Z86.79 (if specified). Don’t report active aneurysm codes unless there is an active lesion.
Audit Red Flags & Best Practice Checklist
Audit Red Flags:
-
Use of I67.1 when documentation does not include “non-ruptured”.
-
Use of I60.x when aneurysm not documented as ruptured, or no hemorrhage documented.
-
Procedure code assigned with root operation “Occlusion” when documentation suggests parent vessel remained patent.
-
Use of unspecified location/side when details were available.
-
Coding a “history of aneurysm” as active without imaging or treatment confirmation.
Best Practice Checklist:
-
Rupture status clearly documented (“non-ruptured”, “ruptured”, “SAH present”).
-
Location (artery name, side) documented.
-
Size and morphology of aneurysm (especially non-ruptured surveillance) documented.
-
Imaging modality and findings documented.
-
Treatment plan or result documented (observe, clip, coil, flow-diverter).
-
Procedure documentation includes objective, device used, approach, parent vessel status.
-
If surveillance/follow-up only, code reflects “history of” rather than active lesion.
-
Coder queries are made when documentation is vague or incomplete.
Summary Table
| Scenario | Diagnosis Code(s) | Key Documentation Needed |
|---|---|---|
| Non-ruptured aneurysm | I67.1 | “Aneurysm, non-ruptured”, location, imaging, plan |
| Ruptured aneurysm with subarachnoid hemorrhage | I60.x (specific) | SAH present, aneurysm rupture indicated, location |
| History of treated/resolved aneurysm | Z86.79 | “History of cerebral aneurysm, treated”, no active lesion |
| Procedure: aneurysm treatment (inpatient) | ICD-10-PCS: root op Restriction (usually) | Objective of procedure documented, method/interface |
Accurate coding of brain aneurysms hinges on the documentation of rupture status, location and laterality, and treatment details or observation plan. For inpatient procedure coding, understanding the objective of the surgery or intervention (whether to exclude the aneurysm while preserving the vessel vs totally occluding it) will guide appropriate root operation selection in ICD-10-PCS.
Training both clinicians and coders on the importance of specific documentation can significantly reduce audit risk, ensure correct reimbursement, and support quality data capture for these high-risk cerebrovascular conditions.