Understanding the Revenue Cycle in Medical Coding & Billing
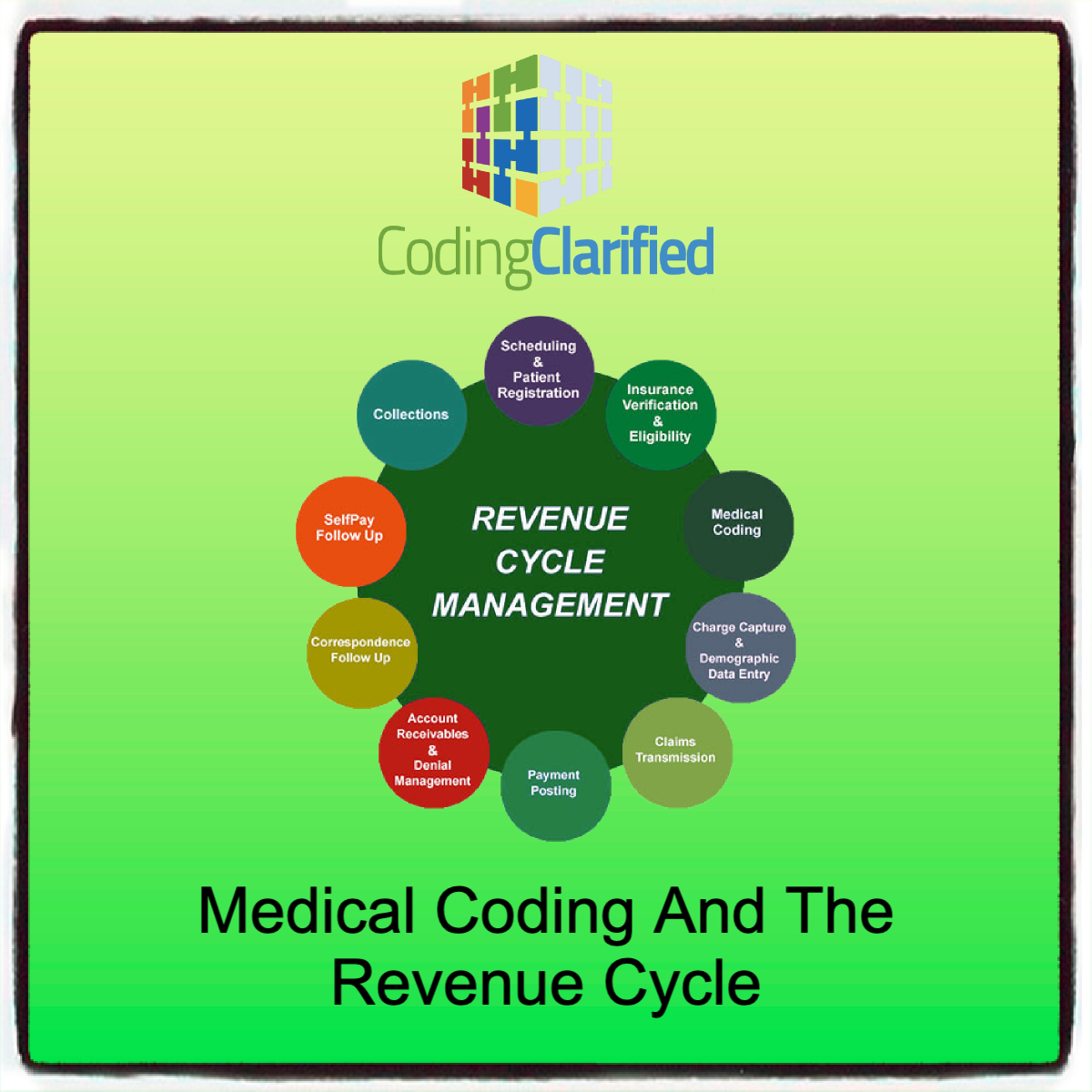
In the healthcare industry, revenue cycle management (RCM) is the financial backbone that keeps a practice or facility running smoothly. At the heart of the revenue cycle are medical coding and billing, which convert clinical services into revenue. Understanding how medical coding and the revenue cycle fit into the larger cycle is crucial for reducing denials, improving cash flow, and ensuring compliance.
What Is the Revenue Cycle?
The revenue cycle refers to the entire process of managing claims, payments, and revenue generation from the time a patient schedules an appointment until the balance on their account is zero.
Key Stages of the Revenue Cycle:
-
Patient Scheduling & Registration
-
Insurance Verification & Authorization
-
Patient Encounter/Service Provided
-
Documentation
-
Medical Coding
-
Charge Entry & Claim Creation
-
Claim Submission
-
Payer Processing & Adjudication
-
Payment Posting
-
Denial Management & Appeals
-
Patient Billing & Collections
-
Reporting & Audits
Where Do Coding & Billing Fit In?
Medical coding and billing are central to converting clinical documentation into revenue. Let’s look at their specific roles:
Medical Coding
-
Translates clinical documentation into standardized codes (CPT, ICD-10, HCPCS)
-
Ensures services are accurately represented for billing
-
Impacts reimbursement based on code selection and medical necessity
Tip: Coders must ensure that codes reflect the level of care and align with payer policies to prevent undercoding, overcoding, or denials.
ICD-10 Steps to Code https://codingclarified.com/medical-coding-steps-for-icd-10-cm/
CPT Steps to Code https://codingclarified.com/medical-coding-steps-for-cpt/
Medical Billing
-
Uses codes to create claims for insurance submission
-
Applies correct modifiers, units, and charges
-
Handles claim corrections, resubmissions, and patient statements
Tip: Billers should follow up on unpaid or denied claims promptly to maintain healthy cash flow.
Why Accurate Coding & Billing Matter in RCM
| Area | Impact |
|---|---|
| Cash Flow | Accurate coding = faster, correct reimbursement |
| Compliance | Prevents audits, penalties, and fraud investigations |
| Denial Prevention | Clean claims reduce rework and delays |
| Patient Satisfaction | Accurate bills build trust and reduce confusion |
| Performance Metrics | Coding drives analytics, benchmarking, and profitability insights |
Common Revenue Cycle Pain Points (and How to Fix Them)
| Challenge | Solution |
|---|---|
| Denials due to incorrect codes | Use coding audits and payer-specific edits |
| Missing documentation | Train providers on required elements |
| Delayed claims submission | Set up daily/weekly claim scrubbing routines |
| High A/R (accounts receivable) | Automate follow-ups and use denial analytics |
| Coding backlogs | Use certified coders and consider outsourcing overflow |
Best Practices for Coders & Billers in the Revenue Cycle
-
Stay Current on CPT/ICD-10/HCPCS updates
-
Use Technology: EHR integration, coding software, RCM dashboards
-
Work Together: Coders, billers, and providers should communicate regularly
-
Audit Regularly: Internal audits catch issues early
-
Educate Providers: Help clinicians understand how their documentation impacts revenue
The revenue cycle is more than just billing—it’s a comprehensive financial ecosystem. Coding and billing professionals play a vital role in its success. By ensuring accuracy, staying compliant, and collaborating with the broader healthcare team, coders and billers help drive efficient, profitable, and patient-centered care.