Guidelines for Medical Coding and Billing for Hepatitis
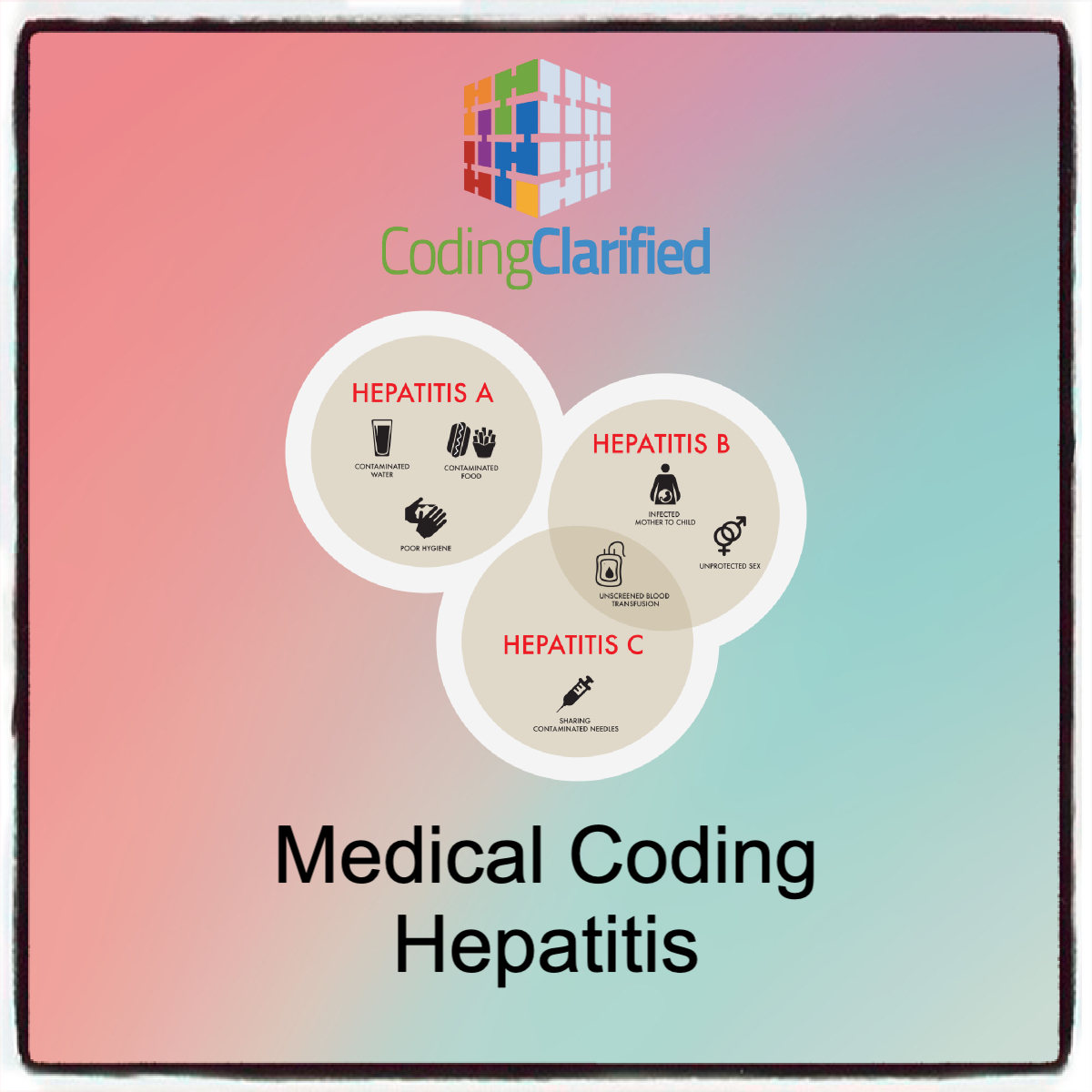
Hepatitis, a medical condition characterized by inflammation of the liver, can be caused by various factors, including viral infections (hepatitis A, B, C, D, and E), alcohol use, medications, or autoimmune diseases. Accurate medical billing and medical coding for hepatitis are essential for ensuring proper reimbursement and compliance with healthcare regulations. The coding process is governed by both the International Classification of Diseases (ICD) and the Current Procedural Terminology (CPT) systems, and must adhere to guidelines issued by the Centers for Medicare & Medicaid Services (CMS) and other insurance providers.
Key Concepts in Billing and Medical Coding for Hepatitis
- ICD-10 Codes for Hepatitis The ICD-10 (International Classification of Diseases, 10th Edition) codes are the primary coding system used to identify diseases and conditions. For hepatitis, there are specific codes based on the type, severity, and any associated complications.
- Hepatitis A (ICD-10 Code: B15)
- Acute viral hepatitis A is coded under B15, which includes categories for unspecified, mild, moderate, or severe cases.
- Code B15.9 is used for unspecified acute hepatitis A.
- Hepatitis B (ICD-10 Code: B16 – B19)
- B16 represents acute hepatitis B, while B17 is used for other viral hepatitis due to hepatitis B (e.g., acute and chronic forms).
- B18 is used for chronic hepatitis B, and B19 covers unspecified hepatitis B.
- Codes also specify whether the condition is in the acute, chronic, or unspecified phase.
- Hepatitis C (ICD-10 Code: B17.1 – B19.2)
- B17.1 refers to acute hepatitis C, while B19.2 is used for chronic hepatitis C.
- Chronic hepatitis C may require more detailed codes, depending on the presence of cirrhosis or liver failure (e.g., B18.2 for chronic hepatitis C with cirrhosis).
- Hepatitis D and E (ICD-10 Codes: B17.9 – B18.8)
- Hepatitis D, a rare form of viral hepatitis, typically occurs in individuals already infected with hepatitis B. The relevant code ranges from B17.9 to B18.8 for various types.
- Hepatitis E is coded under B17.1 and B19.9 for unspecified acute cases.
- ICD-10 Code for Hepatitis due to Alcohol (K70)
- K70.0-K70.9 codes are used to report alcoholic liver disease, including alcoholic hepatitis and cirrhosis.
- Non-Viral Hepatitis (ICD-10 Code: K75)
- This category includes conditions such as autoimmune hepatitis (K75.4) and drug-induced hepatitis (K75.8).
- Hepatitis A (ICD-10 Code: B15)
- CPT Codes for Hepatitis The CPT (Current Procedural Terminology) codes are used for medical procedures and services related to the diagnosis and treatment of hepatitis. These codes typically cover laboratory tests, imaging, and treatment procedures.
- Liver Function Tests (CPT Codes 80076 – 80081)
- These are commonly ordered to assess liver health in individuals with hepatitis.
- Examples include CPT 80076 (Comprehensive Metabolic Panel), CPT 80081 (Liver Function Panel), which includes tests for enzymes such as AST, ALT, and bilirubin levels.
- HCV RNA Quantification (CPT Code 87522)
- This test is used for detecting hepatitis C RNA levels to determine the presence of an active infection.
- Liver Biopsy (CPT Codes 47000 – 47020)
- A liver biopsy may be necessary to assess liver damage or cirrhosis in chronic hepatitis patients. The codes include 47000 (percutaneous liver biopsy) and 47010 (liver biopsy with image guidance).
- HCV Genotype Testing (CPT Code 87901)
- CPT 87901 is used to report the genetic testing of the hepatitis C virus to determine which strain is present, aiding in treatment decisions.
- Endoscopy or Ultrasound Procedures (CPT Codes 43235 – 76942)
- Hepatitis patients may require additional imaging to assess liver status. For example, CPT 76942 is for liver ultrasound.
- Liver Function Tests (CPT Codes 80076 – 80081)
- Modifiers Modifiers are used in medical coding to indicate additional information about a procedure, such as whether the procedure was bilateral, multiple, or performed on an unusual site. Common modifiers for hepatitis-related procedures include:
- Modifier 25: Used to indicate that a separate and distinct procedure was performed during the same visit.
- Modifier 59: Used to indicate that a procedure or service was distinct or independent from other services performed on the same day.
- Documentation Requirements Accurate and thorough documentation is vital to ensure that the proper codes are selected and to avoid denials. The documentation should include:
- Patient History: A complete history of the patient’s condition, including risk factors, family history, and previous treatments.
- Physical Examination: Specific details about any physical symptoms, including jaundice, tenderness, or ascites, which are relevant to hepatitis.
- Laboratory and Imaging Results: Clear results of diagnostic tests like liver function panels, viral load tests, and imaging.
- Diagnosis Confirmation: When applicable, documentation of laboratory or imaging results that confirm the diagnosis of hepatitis A, B, C, etc.
- Treatment Plan: Any medications or interventions prescribed, including antiviral treatments for hepatitis B or C.
- Reimbursement Considerations Insurance providers may have specific requirements for reimbursement related to hepatitis treatment. In general, hepatitis B and C are considered chronic conditions that may require long-term management. Understanding payer-specific guidelines for hepatitis treatment and procedures can help minimize denials. For instance, some insurers may require prior authorization for expensive antiviral therapies or liver transplantation.
- Hepatitis B: Chronic hepatitis B treatment often involves antiviral medications (e.g., tenofovir or entecavir), and insurers may require documentation of viral load and liver function to approve treatment.
- Hepatitis C: Hepatitis C treatment has evolved with direct-acting antiviral drugs (DAAs). Accurate coding of genotype, viral load, and liver damage is necessary for proper reimbursement.
- Billing for Preventive Measures Hepatitis B vaccination (CPT code 90648) is an important preventive measure, especially for high-risk populations (e.g., healthcare workers, individuals with chronic liver disease). Billing for vaccinations should include the proper CPT and ICD-10 codes to identify the patient’s vaccination status and any contraindications.
Medical coding and billing for hepatitis requires careful attention to detail to ensure accurate diagnosis and treatment documentation. By understanding the different types of hepatitis, associated diagnostic codes, and procedures involved in hepatitis management, healthcare providers can ensure that they are properly reimbursed for their services while maintaining compliance with industry standards. Regular updates from organizations like the CMS and the American Medical Association (AMA) are essential to keep up with evolving coding guidelines. Accurate coding and billing help improve the quality of care for hepatitis patients while ensuring financial sustainability for healthcare providers.