Credentialing for Physicians: What It Is, How It’s Done, and Why It Matters
Credentialing is one of the most important—but often misunderstood—administrative processes in healthcare. While coders focus on documentation, code selection, billing, and compliance, physician credentialing ensures that the providers you’re coding for are legally cleared to practice, bill, and be reimbursed. Without proper provider credentialing, even perfectly coded claims will be denied.
Understanding how credentialing works—and how to perform it—is a valuable skill that can open doors in medical billing, compliance, revenue cycle, and practice management.
What Is Physician Credentialing?
Physician credentialing is the process of verifying a provider’s qualifications to ensure they meet the standards required by:
-
Health plans (Medicare, Medicaid, commercial payers)
-
Hospitals and surgery centers
-
Large medical groups
-
Compliance and accreditation bodies
Credentialing confirms that a physician has the education, training, licensure, certifications, experience, and competency to safely practice medicine and be reimbursed for services.
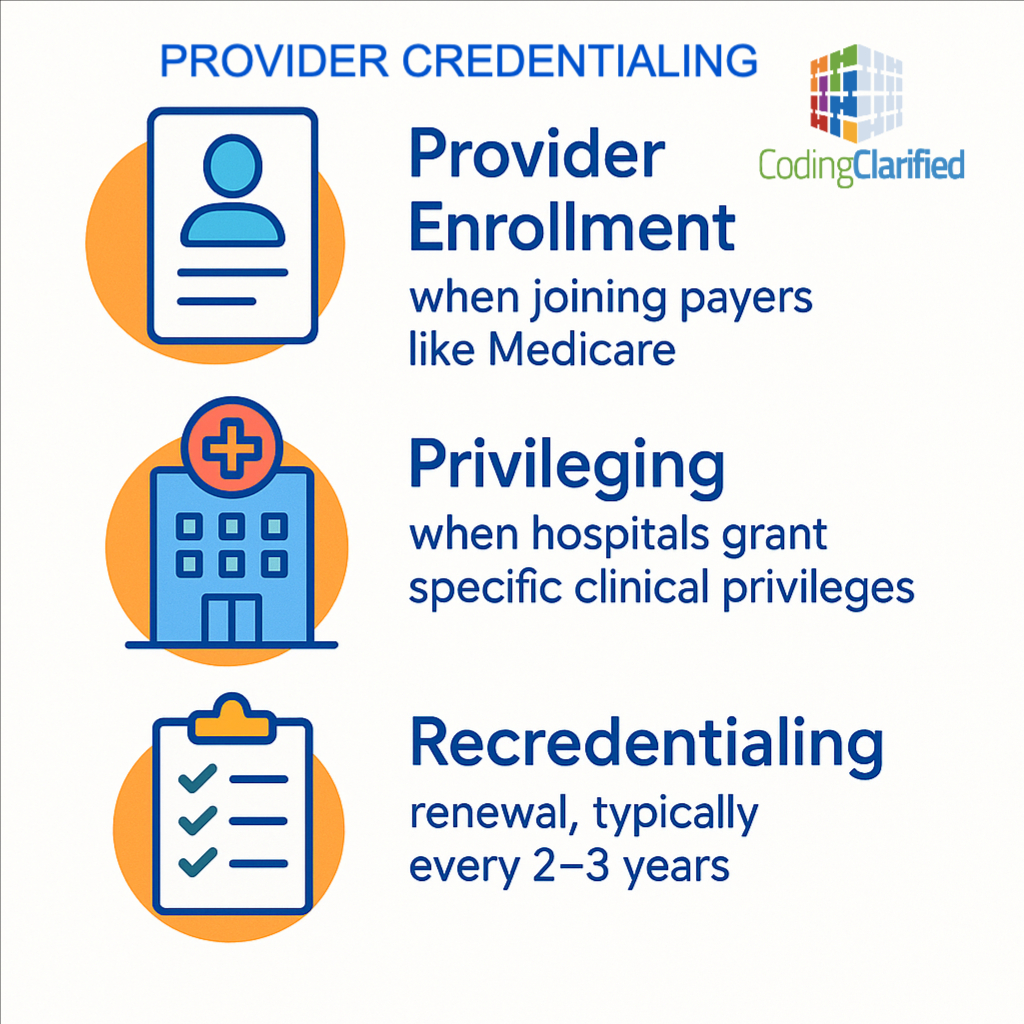
This process is sometimes called:
-
Provider enrollment (when joining payers like Medicare)
-
Privileging (when hospitals grant specific clinical privileges)
-
Recredentialing (renewal, typically every 2–3 years)
Why Is Credentialing Important?
Credentialing protects patients, ensures regulatory compliance, and preserves revenue integrity. Without it:
-
Claims will be denied because the provider is not recognized by the payer
-
Reimbursement will be delayed for months
-
Practices may face compliance issues or even legal action
-
Patient safety risk increases if qualifications aren’t verified
-
Audits and fines become more likely
From a revenue cycle standpoint, proper credentialing keeps providers active, billable, and compliant—making it a critical piece of the healthcare puzzle.
What Does the Credentialing Process Include?
Credentialing requires gathering and verifying a wide set of documents. Common steps include:
Application Intake
Collect provider information and required documents, including:
-
State license
-
DEA registration
-
Board certification
-
Medical school and residency documents
-
Malpractice insurance coverage
-
Work history & CV
-
NPI (National Provider Identifier)
-
CAQH profile (must be kept updated)
Primary Source Verification (PSV)
This ensures all credentials are validated with the original source, such as:
-
Medical schools
-
Licensing boards
-
Certification bodies
-
AMA profiles
-
NPDB (National Practitioner Data Bank)
Payer Enrollment
The provider must enroll individually with each payer they plan to bill:
-
Medicare PECOS enrollment
-
Medicaid enrollment (state-specific)
-
Commercial payer credentialing portals
Hospital Privileging (if applicable)
Hospitals review training and experience to determine which procedures the provider can perform.
Final Approval
Once approved by the payer or facility:
-
The provider receives an effective date
-
The practice can begin billing
-
The provider is added to rosters and directories
Recredentialing
Typically required every 2–3 years. Failure to maintain results in claim denials.
How Long Does Credentialing Take?
Timelines vary by payer:
-
Medicare: 45–60 days
-
Medicaid: 60–120 days
-
Commercial payers: 60–180 days
-
Hospital privileging: Up to 90 days
This is why credentialing must start early—ideally 2–3 months before a new provider begins seeing patients.
How Can You Learn to Do Physician Credentialing?
The good news: Credentialing is a high-demand skill and pairs well with medical billing/coding knowledge.
Ways to learn credentialing:
On-the-job training
Many coders and billers learn credentialing by working in:
-
Private practices
-
Provider enrollment departments
-
Revenue cycle teams
-
Healthcare staffing/locum agencies
Online credentialing courses
Look for training in:
-
Provider Enrollment
-
CAQH Management
-
Medicare PECOS
-
Payer Contracting
-
Credentialing Compliance
Practice with credentialing portals
Hands-on experience makes the biggest difference:
-
CAQH ProView
-
Medicare PECOS
-
Payer enrollment portals for Aetna, UHC, Cigna, etc.
Learn healthcare compliance
Credentialing is closely tied to:
-
CMS regulations
-
OIG guidance
-
NPDB requirements
-
State licensing rules
Join professional associations
Organizations like NAMSS (National Association Medical Staff Services) offer:
-
Certification programs
-
Networking
-
CEUs
-
Resources and best practices
Tips for Success in Provider Credentialing
Stay organized
Create checklists, track expiration dates, and build a credentialing calendar.
Keep CAQH updated
It is a primary source for most payers—expired documents cause delays.
Monitor expiring credentials
Licenses, DEA, board certifications, malpractice insurance, and hospital privileges all have expiration dates.
Communicate clearly with providers
Physicians are busy—credentialing moves faster when they respond quickly.
Know each payer’s requirements
Every insurer has unique forms, timelines, and approval processes.
Document everything
Audit trails are essential if payers question application timelines or requirements.
Follow up consistently
Payers are slow. Your follow-up is what keeps applications moving.
Why Credentialing Knowledge Helps Medical Coders
Most coders focus on documentation and coding accuracy—but knowing credentialing strengthens your role because:
-
You understand why a claim denied due to “provider not credentialed”
-
You can help prevent avoidable reimbursement delays
-
You become more valuable in small practices and revenue cycle teams
-
You can expand your career into provider enrollment, management, or compliance
-
You gain a competitive edge in hiring because most coders do NOT know credentialing
This knowledge makes you a stronger asset to your employer and elevates your professional versatility.